June 16, 2022
Facebook Live: The Reverse Alzheimer’s Summit 2.0

In this Facebook Live, Dr. Dale Bredesen was joined by Marama founder Dr. Heather Sandison, and they discussed the upcoming virtual Reverse Alzheimer’s Summit 2.0 to be held June 14 to 21. Additionally they shared an in-depth preview of the information that will be shared by the over 40 dementia and aging experts at the summit. Register for free by clicking on the button below.
Dr. Bredesen and Dr. Sandison discussed the actionable information you can take now for brain optimization and how to identify, prevent, and treat cognitive decline. Dr. Sandison shared some of her successes with residents of Marama and how her patients provided her with the inspiration to share this valuable information and host this summit.
For your convenience, we have included the full recording and the transcript below.
Watch here:
Transcript:
Dale Bredesen (00:00): Good day, everyone. And welcome to Facebook live. I’m here with Dr. Heather Sandison. Heather, great to have you as always. Thank you so much for joining us.
Dale Bredesen (00:00): Good day, everyone. And welcome to Facebook live. I’m here with Dr. Heather Sandison. Heather, great to have you as always. Thank you so much for joining us.
Heather Sandison (00:09): It’s a privilege to be here.
Dale Bredesen (00:11): Heather, you did a tremendous job with Reverse Alzheimer’s Summit 1.0 and now you have a second one coming up. Could you tell all of us a little bit about how you got into treating patients with cognitive decline and then a little bit about how you decided to do a Reverse Alzheimer’s Summit? I think it’s been extremely successful and certainly lots of great comments about it.
Heather Sandison (00:32): Thank you. So originally, I came to a lecture of yours in 2015, 2016, and I heard that you could reverse Alzheimer’s. I was of course a bit skeptical because I had been told over and over again, that to tell someone that you could reverse their dementia was to give them false hope.
Dale Bredesen (00:51): Right.
Heather Sandison (00:51): And that wasn’t realistic, and it wasn’t responsible as a medical provider. But I was intrigued by what you had to say at that conference, because what you were saying was that if we took this comprehensive approach, if we did everything we could to reduce the inflammation, the infections, if we replaced hormones, if we got on a great diet, if we increased exercise, all of these things that made so much sense to me, if we put them all together, we stacked them all, that you had seen that people could reverse their dementia and regain their cognitive function.
Heather Sandison (01:25): So, I was very intrigued. It made sense to me as a naturopath. So, I went to your training. And after the training, I was on your list of Bredesen trained providers. So, I had patients who were less skeptical than me, very enthusiastic, who did me the honor of serving as their provider and supporting them in the ways that I could early on in this process.
Heather Sandison (01:48): My first patient, her name is Linda, came in with a MoCA of two out of 30. We know that a perfect MoCA score is 30 out of 30. You want to be above 24 to be normal. And then when you’re at two, this is severe decline. This is severe disease. This had affected her handwriting. She could barely answer with even yes or no responses to questions. I could see that she could sometimes understand the question, but she couldn’t even deliver a full sentence.
Heather Sandison (02:18): Of course, this had affected her relationship with her husband, and they were ready. They were to do ready to do whatever it took to get her back. And so, they did. I saw her six weeks later and her MoCA was a seven. Even telling that story today gives me chills because it was so profound. Of course, my first thought was, what did I do wrong? Did we measure it wrong the first time? Yeah. Note, her husband confirmed, she did a different person.
Dale Bredesen (00:00): Good day, everyone. And welcome to Facebook live. I’m here with Dr. Heather Sandison. Heather, great to have you as always. Thank you so much for joining us.
Heather Sandison (00:09): It’s a privilege to be here.
Dale Bredesen (00:11):Heather, you did a tremendous job with Reverse Alzheimer’s Summit 1.0 and now you have a second one coming up. Could you tell all of us a little bit about how you got into treating patients with cognitive decline and then a little bit about how you decided to do a Reverse Alzheimer’s Summit? I think it’s been extremely successful and certainly lots of great comments about it.
Heather Sandison (00:32): Thank you. So originally, I came to a lecture of yours in 2015, 2016, and I heard that you could reverse Alzheimer’s. I was of course a bit skeptical because I had been told over and over again, that to tell someone that you could reverse their dementia was to give them false hope.
Dale Bredesen (00:51): Right.
Heather Sandison (00:51): And that wasn’t realistic, and it wasn’t responsible as a medical provider. But I was intrigued by what you had to say at that conference, because what you were saying was that if we took this comprehensive approach, if we did everything we could to reduce the inflammation, the infections, if we replaced hormones, if we got on a great diet, if we increased exercise, all of these things that made so much sense to me, if we put them all together, we stacked them all, that you had seen that people could reverse their dementia and regain their cognitive function.
Heather Sandison (01:25): So, I was very intrigued. It made sense to me as a naturopath. So, I went to your training. And after the training, I was on your list of Bredesen trained providers. I had patients who were less skeptical than me, very enthusiastic, who did me the honor of serving as their provider and supporting them in the ways that I could early on in this process.
Heather Sandison (01:48): My first patient, her name is Linda, came in with a MoCA of two out of 30. So, we know that a perfect MoCA score is 30 out of 30. You want to be above 24 to be normal. And then when you’re at two, this is severe decline. This is severe disease. This had affected her handwriting. She could barely answer with even yes or no responses to questions. I could see that she could sometimes understand the question, but she couldn’t even deliver a full sentence.
Heather Sandison (02:18): Of course, this had affected her relationship with her husband, and they were ready. They were to do ready to do whatever it took to get her back. And so, they did. I saw her six weeks later and her MoCA was a seven. Even telling that story today gives me chills because it was so profound. Of course, my first thought was, what did I do wrong? Did we measure it wrong the first time? Yeah. Note, her husband confirmed, she did a different person.
Heather Sandison (02:48): When I saw what was possible for Linda, how I’m sure for you, it was the same. When I saw what was possible, I thought, how could I do anything, but dedicate my life to this and tell everyone that they’re wrong, that there is hope, that there are so many things that you can do. Not only is there not nothing you can do and that’s factually inaccurate, but it’s almost overwhelming how much you can do to support cognitive function.
Dale Bredesen (03:13): It’s a great point. As we’re all learning and as we have a bigger and bigger community, we’re seeing what’s the priority? What are the things that are really critical? What are the things that are less critical? So, you’ve done obviously a number of really innovative things. One of the things of course is to set up the first Reverse Alzheimer’s Summit. And what gave you the idea? So, you were going along seeing patients, and at some point, you decided to put on a summit. How did you get the idea for that?
Heather Sandison (03:41): I had people, patients coming into my office saying, “Well, my neurologist told me there was nothing I could do? I heard that enough times and I was just thinking like, “What is the way to get the word out? How can I do this? How can I spread the word more that there is something you can do?” And also give people answers about what it is that you can do, right? Get the experts involved and show that there is a deeper, bigger conversation going on that’s aiming to reverse this narrative about there being nothing that can be done or that’s only a one-way downhill slide.
Heather Sandison (04:15): So, the summit came up as an option just in my networks of other doctors. They said, “If what you want to do is change the conversation, then start a new one.” A summit is a great way to get the word out. It’s also free. So there’s lots of conferences. You’ve written some incredible books. I didn’t have access to a publisher at that point. So that wasn’t quite the option that was available to me. What I love about the summit is that they are free. They’re so accessible. You don’t have to fly anywhere. You don’t have to know anyone, you just sign up with your email and then you get access to all of these talks, all of this really great information that I hope we’ve created and curated in a way that people can take this information and start implementing immediately and start to hopefully see changes.
Dale Bredesen (05:04): Yeah. That’s a really good point. And obviously, the first one was very well received. So you’ve now got the second one coming up. Could you tell a little bit about some of the different topics that people are going to talk to and also about the specific dates and what’s the best way for people to access it
Heather Sandison (05:22): Yeah. I know that the link should be in the chat here. It’s the Reverse Alzheimer’s Summit 2.0 2022 version. And day one, we’re going to talk about big picture things. This is June 14th, so right around the corner. Just next week, this starts. So, get signed up now. All you have to do is go to the site, plug in your email address, and then you will start getting emails confirming that you’re registered. And then you will get emails starting on the 14th, saying, “Click here to log in and you’ll be directed to all of the talks.”
Heather Sandison (05:53): On day one, all of the talks for day one will go live all at once, so you can watch them at your leisure throughout the day. And we’re going to talk again, like big picture ideas. So, this is the day our conversation is going live, my conversation with Dr. Perlmutter. Some of the big thinkers in this space.
Heather Sandison (06:09): Also, we’ll take a look at what the research is doing. What have we learned in the past year since we have had the previous one? What are the updates? Also, talk about the import importance of health coaching. We know that part of this, as you mentioned, we want to know what the big impactful things are. What’s the 80/20 on this? Also, this is a long-term neurodegenerative process. It doesn’t happen overnight. And what I’ve seen clinically is that the more comprehensive we can be in applying the whole protocol, the Bredesen protocol, your approach, the more confidence I have in getting results.
Heather Sandison (06:44): So, having things like Apollo, the amazing work you guys do at Apollo, having the ReCODE Protocol™, having health coaches involved, we want to talk through some of that on day one. How do we logistically set this up to get the most out of it? And then-
Dale Bredesen (07:01): Gotcha. Go ahead.
Heather Sandison (07:03): Let’s talk a little bit more about that. I’d love to hear your thoughts.
Dale Bredesen (07:06): Please continue. Go ahead.
Heather Sandison (07:08): Then day two, we get into … From my perspective, I was sharing with you a little bit before we jumped online, we forget … At times it’s easy to forget the humanity when we’re stuck in the labs. What is it that’s wrong? How do we fix it? What do we take? That can be sometimes distracting from just the conversations and just being present with your loved one who’s suffering with dementia. There are skills that we can build in terms of communication. Teepa Snow is someone who I invited to be on and interviewed.
Heather Sandison (07:40): She is just a wealth of knowledge in terms of simple tricks that you can use day to day if you’re communicating with someone who has dementia. We also talk on day two about how stressful it is to be a caregiver and how caregivers are at higher risk for developing dementia later on in their life. So, we want them to put their oxygen mask on first and we talk through a lot of the … Again, like the skill building or the coping mechanisms that can help us with that.
Heather Sandison (08:07): So, day two is really around stress and lifestyle management of those stressors and how much of an impact that can have on the brain. Day three, we talk about toxins. So this is your type three Alzheimer’s. We do deep dives into heavy metals, mycotoxins, and the chemical toxins.
Heather Sandison (08:26): Stephanie Seneff is chatting about glyphosate and other chemical toxins. We’ve got mold experts like Neil Nathan, Margaret Christensen. Some of the biggest names in mold illness are with us that day. And then Chris Shade, who I know taught with your group on the ReCODE 2.0 Training, he teaches a lot of doctors about how to get heavy metals out. So, you’ll learn from some of the experts in toxicity on day three.
Dale Bredesen (08:51): Fantastic.
Heather Sandison (08:52): Day four is diet. You asked me what I think is one of the most critical pieces of this approach of the ReCODE protocol, and I would say that ketogenic diet.
Dale Bredesen (09:05): Yeah. I absolutely agree. People who are not doing well are typically not getting into ketosis. And the people who are doing well are typically getting into ketosis. And the people who are having a little problem are the ones that are saying, “Well, I’m trying to get into it, but I’m not there yet”. So that’s actually one of the important things that comes up again and again. If it’s critical to have the ketones, then I like the idea of just starting with some exogenous ketones, making it easy for people just as Professor Steven Cunnane has shown us, you can bridge that energy gap. And then over time, sure, get into endogenous ketosis.
Dale Bredesen (09:43): But especially for people who are frail and who are underweight, they can actually be hurt by trying too hard to do endogenous ketosis. I think you make a really good point. That is a critical, critical variable to get best outcomes.
Heather Sandison (10:00): We have some great people talking about how to get into ketosis. And then of course, Terry Wall is one of the greats in neurology who reversed her own neurodegenerative disease, MS. She is interviewed that day. Kara Fitzgerald, a naturopathic colleague of mine who has published, published research on reversing your aging clock. She talks about the diet that she uses to make yourself younger. And then Max Lugavere, who also talks widely about changing your diet for brain health. And then Amy Berger, who also is published extensively. And West, you interviewed West that day. So, we’re talking a lot about the nutrients and I hope again, giving people really practical tools and ideas for good healthy meals so that they can switch to a really brain healthy diet, whatever that means for them.
Dale Bredesen (10:56):
It’s a really good point. And then again, one of the paradoxes here is that if you look at back at the test tube and you look at what this disease actually represents, the fundamental concept, it really looks like a network insufficiency. So, you have this beautiful neuroplasticity network. And as you said, it has nutrients and hormones, trophic factors, and it has inflammation that affects it. It’s got toxins that affect it, and energetics, mitochondrial, on and on. But at its heart, it is a neuroplasticity network, and you are downsizing it when you aren’t supporting it. Or when you’re demanding too much from it with things like inflammation.
Dale Bredesen (11:36): On the one hand, you want to get those ketones. At the same time, the fasting part helps you to become insulin sensitive. And you really need both. You need you to have the insulin sensitive, but you also need to be able to have ketones and use ketones whether you’re making them yourself or whether you’re taking yourself. And I think that’s something that people often have trouble with because they’re either doing too much fasting and just losing too much weight, or they’re just relying on the exogenous ketones, and they still continue to have the insulin resistance, which is also a problem. If you can get those two things balanced, it is really critical for optimizing the support, your energetic support.
Heather Sandison (12:18): Absolutely. Diet is just so foundational, right? There was a trial, I’m sure you saw it, out of Florida. They published it in just January of 2020. It’s a feasibility trial. So very small. Just nine or ten patients, but in just six weeks of ketosis, there was a measurable statistically significant, even with this small group, a measurable change in cognitive status improvement. And just six weeks, and I think some people lose sight of the fact that you don’t have to be in ketosis forever. That’s not the idea.
Heather Sandison (12:51): But if we can get someone in ketosis for three, they become keto adapted, much more metabolically flexible, and they get those cognitive benefits. I love being in ketosis personally because I feel like I get another hour and a half in my day. I wake up ready to go. I don’t struggle to get out of bed. I have so much more energy. It’s so much more balanced. Like you and I both, we stay busy. And having that extra hour in my day is so, so valuable as well as just turning my brain on. I personally get so many benefits, so hope that other people are inspired to get those benefits as well.
Dale Bredesen (13:28): Absolutely. Fantastic. And then let’s talk about the end of the conference. How do you end there and then how do people access it?
Heather Sandison (13:36): Yeah. Day five, we’re going to be talking about structural things. So, this is traumatic brain injuries, oral health and airways, the sleep apnea, the value of sleep, the value of exercise and what types of exercise are best for the brain. Also, genetics and how genetics can impact our risk for dementia. So that’s on day five. And then day six, we’re focused on the ladies because women are affected so much more frequently than men are by this awful disease, both as patients, but also as caregivers.
Heather Sandison (14:13): So (we need to make) sure that women have the support they need, that they understand the hormones. There’s always lots of questions about keto and lots of questions about hormones. We want to make sure people really understand and feel empowered about their hormonal health as they age. We have an amazing lineup of ladies talking about that.
Heather Sandison (14:32): And then day seven, we go into is some of … Super exciting for me. It’s like the growing edge of all of this research, peptides, plasmapheresis, laser therapies, oxygen therapies. We really dig into like what’s on the cutting edge of reversing dementia where maybe there isn’t quite enough research for us to say that everyone should be doing this, but things like stem cells where there’s probably a lot of great benefit and yes, it needs more research. Yes, the cost needs to come down, but we still want to understand if we were hacking this and throwing everything at it, what are those conversations looking like?
Heather Sandison (15:11): So that’s day seven. And then what we’ll do is this is free. Each of these days are free for the days that they’re live and that’s the 14th through the 21st of June. And then that following weekend, everything is going to be available.
Heather Sandison (15:26): If you’re signed up, there’s an Encore weekend and this is … Nobody else knows about this. So, I’m just telling everyone who’s present right now that encore weekend will be available. If you are traveling, if you’re on summer vacation from the 14th to 21st of June, don’t worry. That next weekend, you’re going to have access to all of the talks from every single day. And if you’re out of town for all of June, there is an option to purchase.
Heather Sandison (15:52): For just $67, you can purchase all of the recordings for the entire summit. That price will go up between now and when the summit ends. So, make sure you get in there. If you don’t feel like you’re going to have a chance to watch all of them or get the benefit of this while it’s free, then I hope that it feels like a pretty good price to get access to all this information.
Dale Bredesen (16:12): Yeah, certainly not prohibitive. And again, as you said, you can do it for free if you want to. So, there’s a tremendous amount of access. You’ve really brought together all of the different pieces that are so critical. Everything from the fact that it’s a woman centric disease as Maria Shriver has pointed out for years to the fact that you’ve got some of the latest, greatest. What are the things that are coming? What is just over the next hill, to how does this work and what are the critical pieces? And interacting with people, I think this is fantastic. Very exciting.
Dale Bredesen (16:44): Now, couple of other things I wanted to ask you about, because you’ve really done so many exciting things in this field. One of the things you did a few years ago is to set up, Marama, which is, as far as I know, it’s first of its kind. Very exciting for us to see that people actually have an option when they’re looking for assisted living. They don’t have to go and eat horrible food and do nothing but go downhill because so many of us as we see people go into assisted living, we see them fall off the cliff. I think Marama is such a fabulous idea and really fulfills a niche. So, could you talk a little about it? Of course, Lance and I were there at your opening, but I’d love to hear where things stand now and where are things going with Marama.
Heather Sandison (17:30): It was so, so, so special to have you guys there. Thank you for joining us for that celebration. It happened the week before the world shut down. For better or worse, it was good timing. Marama happened because I had been seeing patients that were sent through you after I did the training and I saw them getting better. I developed a bit of a reputation, like, “Okay, I was the one in San Diego doing this.”
Heather Sandison (17:56): I started getting emails from people saying, “Hey, my uncle or my dad, or my mom, they have this disease. I’m aware of the Bredesen protocol. I’m aware of this approach. I really want them to do this. And I’ve got my own kids and I’ve got a job, a full-time job. I’ve got managing my house and I can’t drop everything to make this happen for them. Where should I send them? Where can I send them where they can get the benefits of the ReCODE protocol of this Bredesen approach, and I don’t have to sacrifice my entire life.
Heather Sandison (18:26): So, I looked around and in this was in 2019. I couldn’t find anywhere that I felt confident sending people. There were some places incorporating saying like, “We’ll take you to a Bredesen-trained doctor and we’ll help you with the supplements.” But there wasn’t a place that was offering a ketogenic diet.
Dale Bredesen (18:44): Oh my gosh.
Heather Sandison (18:45): As you know, if I’m sitting next to someone who’s having cake and cookies and I’m supposed to only eat my carb-free diet, I’m going to want those cake and cookies so much more because I feel deprived. But we can make amazing, satisfying, wonderful ketogenic food, and that’s what we do at Marama now. And everybody is on the same plan. So, you don’t have that temptation. You don’t forget, right? Most patients with dementia, they forget what they’re supposed to eat and not supposed to eat.
Heather Sandison (19:15): When I saw that there wasn’t a place doing it that I really felt like I could emphatically recommend, I thought, “Well, how hard could it be?” And Dr. Bredesen, really this work chose me. I never imagined this would be the work that I would be doing ten, 15 years ago. One thing after another has led me to doing this with relative ease. Don’t get me wrong. It’s not always easy. Of course, it’s a hard approach. And yet things have lined up for me over and over again so that I can make this available.
Heather Sandison (19:46): I very much feel I’m living my purpose. Even meeting you was very serendipitous. So, I feel super fortunate that I have been able to create Marama. We have a wait list right now and so we’re looking for a second location. We’re very excited to expand.
Dale Bredesen (20:07): I can’t tell you how many times I’ve had questions of, I’m in New York city, or I’m in Texas, or I’m in Miami, or I’m in Omaha, where’s the Marama near me?” So many people now know about Marama and wish that there were a Marama right near them. I think it’s a huge hit and it’s just a wonderful, wonderful idea. And to see you really bring it to fruition because it’s not easy. I mean, you minimize the work, but this is a tremendous amount of work to bring a new concept to fruition over time and get the support to do it, get the team to do it, get the advertisement to do it, make sure it’s done right. Get the results.
Dale Bredesen (20:53): I mean, that’s not easy. So, congratulations. That’s just such a fantastic accomplishment. I hope there will be 200 Maramas at some point around the world because that’s really what the world needs.
Heather Sandison (21:06): And you’re actually right. We get calls from Australia and Japan, and Switzerland. This is a disease that affects people all over the world. And my success for me would be that the entire senior living industry changes. And if somebody is looking for a place to send their mom or their loved one, when you call, ask them, “Do you provide a brain-healthy diet? Are you familiar with the Bredesen protocol? What does exercise look like at your facility? How many TVs are in the rooms? Just asking these questions as consumers, as someone that might potentially be in charge of that decision-making around where your loved one lives, just asking those questions is going to get that industry to change. And we need it to change. They are not serving our seniors and the way they could be.
Dale Bredesen (21:54): Yeah, it’s true. And of course, the argument we hear often is that, well, I’ve given up and I just want to eat hot fudge Sundays. There’s nothing wrong with that. If someone wants to give up, but if so many times the person hasn’t given up and they really want to continue and do whatever they can. So having a place like Marama is just such a blessing. You’ve done a beautiful interview before talking about people you’ve seen get better at Marama. Maybe if you could just give us one example of someone you’ve seen where you felt that the outcome was very positive.
Heather Sandison (22:25): Yeah, absolutely. There’s a bunch. So, Jan moved in May of 2020, her and her husband and they are just a delight. And when she first moved in, she had severe short term memory loss. She couldn’t remember what you had said 10 minutes earlier. She repeated questions, repeated stories. I think many people can relate to having conversations like that with their loved ones. When they’re not fully there and very confused about, “Oh, what is this for dinner?” Even though it seems like it’s very clear that it’s salmon or whatever it was.
Heather Sandison (22:56): Now, she could probably live independently. She no longer has short term memory loss. She will finish your sentences for you. I was over there recently and there was a new gentleman moving in, I guess it’s not that recent anymore. But there was a new gentleman moving in and I couldn’t remember his name. There’s a lot going on. I was there for dinner with the residents, and I was like, there’s an … I was telling them all. So, on Monday he’s showing up and his name is, and she saw me pauses and she said, “Norman.” She was a hundred percent right.
Dale Bredesen (23:29): Wow.
Heather Sandison (23:31): She’s finishing our sentences. Her daughter notices on the phone when they chat. She says, “Oh yeah. Mom is telling me. I’ve already told her that. I don’t need to tell her again. So, it’s really fun to see. Her husband, he is doing much better as well, but he’s not ready to live independently. So, they’re going to stay at Marama. They’ve been there a couple of years now. And what was surprising to me, I don’t know why I was surprised, but they continue to get better.
Dale Bredesen (23:57): Yeah. Isn’t that exciting?
Heather Sandison (24:01): She continues to get better. And in surprising little ways, just being more independent with her activities of daily living. She used to need more help in the shower. She doesn’t anymore. So she’s gotten stronger, more stable. It’s really an absolute privilege to watch just miracles happen. We had another resident who was on hospice earlier this year and we threw everything out at IVs and stem cells and all of it. And her loved ones are so committed, and she is just a miracle. The IV doctor was over there a few weeks into this, and the resident grabbed her hand and looked her in the eye and said, “Thank you.” So really …
Dale Bredesen (24:48): That is fantastic. As we’ve seen, it chokes up the doctor just to see these amazing things that I remember when one of the doctors saw the very first person getting better, who happened to be an anesthesiologist. She wrote that the guy came back in and was better and she started crying, not just the patient. It’s great to see when you have somebody that is impossible to treat. What’s really intriguing to me is the fundamental research that we did in the lab for so many years has to fit with what you see clinically.
Dale Bredesen (25:27): The clinical work teaches the research. The research teaches the clinical work and they kind of move together. And if something doesn’t make sense, you have to go back to the drawing board. Now, what you just described with continuing to get better, these people are in a synaptoblastic side of the signaling pathway. So over time, they should continue to be able to make synaptoblastic signals to create and utilize and maintain new synapses.
Dale Bredesen (25:59): So that’s really fantastic to hear, and it just absolutely fits beautifully. And of course, this brings up the next thing, which is that so many people … I was just on a podcast this morning and the interviewer said, “I’ve never heard of people getting better with cognitive decline.” And like, “Well, yeah. It’s published. We have a pre-print out there. We now have a piece that’s in press on the trial where about 80% of the people actually got better.”
Dale Bredesen (26:26): I know you’ve got a trial that’s going to be coming out. Could you give us … I know it’s not published yet, so I know you can’t tell us everything, but if you could just give us a little thumbnail about how you did this trial and what you saw in the trial.
Heather Sandison (26:39): Yeah. Again, I was seeing people getting better in my clinic and I was very fortunate to have a patient who was a philanthropist. And he said, “How can I help?” And I was like, “Wow, you could pay off my student loans.” But instead of saying that, “I thought, what would be more helpful for everyone?” And that is learning and measuring and learning. There’s a criticism I think of what you and I do. And it’s that there’s not enough research. And that’s valid. There isn’t enough research. We need so much more data to really understand.
Heather Sandison (27:10): Like you’ve said, what are the most critical components of a complex protocol? How do I tell someone how likely it is that they’re going to get better if they do parts of it, or if they do all of it? I was getting that question often enough. If I spend the money, if I spend the effort and the time, if I get hopeful about my loved one getting better, how likely is it that we’re going to see results?
Heather Sandison (27:32): I didn’t know the answer to that. Your paper wasn’t out yet. And I think you and I were having similar thoughts of like, “All right. How can we put together at least a small feasibility trial?” So, we took 25 participants, and they went from MoCA scores … They had measurable cognitive impairment. MoCA scores of 12 to 23.
Dale Bredesen (27:51): Wow.
Heather Sandison (27:52): We took them through six months of my version of your protocol. So aggressive treatment, getting toxins out, getting nutrients up, like ketogenic diet. Lots more exercise and different types of exercise. Walking isn’t enough. And getting them out of moldy environments, all of the nutrients. Just throwing all of it at it. What we then measured was EEG data, MoCA scores, of course, and then we used the Cambridge brain sciences, their battery of cognitive testing. I’m very excited to share those results with everyone.
Heather Sandison (28:30): Actually, one of those patients was here this morning. She brought her son because one of the big applications of this is that the next generation shouldn’t have to suffer, right? If we can [inaudible 00:28:42] identify risk, then this can be an optional or rare disease. So, she was here. She’s an APOE 44. So, she has two copies of the 4/4 status (allele), and she had measurable cognitive decline a year and a half ago or so when we got her enrolled in the study. And she is doing phenomenally well. Her MoCA score is a 30 out of 30. She has fully recovered.
Dale Bredesen (29:07): Wow.
Heather Sandison (29:10): She has her life back. I’m here in Southern California. She was an avid surfer. She had lost interest in surfing. She was struggling to get up and out of bed in the mornings. She was depressed because she couldn’t engage. She was withdrawing from her friends. She was more dependent on her children. It was really sad, and she was very scared. She has a dad who is in the end stages of Alzheimer’s. So now she feels very empowered. She’s got her life back and she’s fully cognitively functional and she’s now helping her kids make sure that they prevent this from ever being an issue for them.
Dale Bredesen (29:45): Yeah. That’s just fantastic. So exciting. That’s wonderful. Okay. We’ve got some excellent questions here. Let’s go through these questions. And here is from Sajid who says, “Please talk about neurofilament blood tests. Everyone is interested in can we measure this more easily?” The idea of doing a spinal tap. I mean, who wants a spinal tap? And this is really kind of becoming a thing of the past, but there were a lot of measurements made in spinal fluid. Then of course, PET scans, which are extremely expensive. And so, everyone has been after, can we get an accurate blood test? And one that is early.
Dale Bredesen (30:23): I think that’s an important point to emphasize. This disease has been diagnosed in the very late stages for too many years. You’re past the first stage, which is you’re pre-symptomatic. You’re past the second stage which is subject to cognitive impairment. Often past the third stage, mild cognitive impairment.
Dale Bredesen (30:41): And then you’re all the way into the fourth and final stage, which is dementia. We really need to get just as we look for insulin resistance, we need to look for pre-Alzheimer’s much more. So yes, neurofilament has been used. It was used a few years ago for looking at patients with ALS. So, you have to be a little careful. It is associated with neural damage, but there has been some interest in using this in Alzheimer’s as well. And Heather, is that one of the markers you’ve used or not?
Heather Sandison (31:08): I haven’t used that. My question is always, why is there decline happening?
Dale Bredesen (31:15): Yes.
Heather Sandison (31:16): And looking for beta-amyloid plaques or tau proteins, they’re doing imaging to measure. It doesn’t give me as much information about the why. Although, I think it gives us information, right? A picture speaks a thousand words. I know that in your trial, you guys measured MRIs and you showed that you were getting increasing gray matter. Right? Did I get that right?
Dale Bredesen (31:37): Yep.
Heather Sandison (31:37): Increased hippocampal volume. And that is so powerful in terms of the story it tells. And yet for me as a clinician, I kind of go, “Yeah, but of course. But what really matters is your cognitive function. Are you more functional in the world?” And that’s what I tend to measure. But these tests are … I’m a data person. So I’m all about it. If we can do them, let’s do them. But I have not used that one yet.
Dale Bredesen (32:05): Yeah. And again, more is going to be coming. There’s Phospho-tau217 which is out now. There will be phospho-tau181. There is A beta 42 to 40 ratio that has been used. So, I think more and more we’re going to get a much better look at people. As you say, the problem with these is that they’re downstream. We want to know why. And I think the epigenetics are going to do a better and better job at saying, “Okay, here are the things that are actually driving this process.”
Dale Bredesen (32:31): I know you’ve interacted with Dr. Pither from England. Actually, I talked to him extensively just a couple of nights ago, and they’re heading toward that kind of actionable. They’re really slightly started with using the polygenic risk score. But they’re now also heading toward more of a functional medicine actionable set. And of course, there’s IntellxxDNA from Dr. Sharon Hausman-Cohen. Also, tremendous amount of actionable information.
Dale Bredesen (32:58): So, I think we’re getting a better and better understanding with each patient about what’s actually driving the problem and therefore what we can do about it, which is, I think it’ll give us better and better outcomes in the upcoming years.
Dale Bredesen (33:11): And then here is from Marie, who says hello from Iceland. Hello, Marie. Says, “I have sporadic fatal insomnia since 2017, supporting with doxycycline and some supplements. Could you please help?” So yeah, what I would recommend, please, you need to have an additional evaluation, et cetera. At what are the things that might be contributing? Now, to be fair, this is a prion disease where PRP is involved.
Dale Bredesen (33:37): It is different fundamentally than Alzheimer’s. However, PRP and APP do interact. So, you might consider going to Cognition, which is in Edinburgh and talk to the physicians there. I think they’ve done a very nice job with a number of patients.
Dale Bredesen (33:55): Next here is from Anna. What medicine can I use for my mother’s myoclonus with Alzheimer’s. Myoclonus is not terribly common with Alzheimer’s. I don’t know, Heather, have you seen myoclonus in your patients with cognitive decline?
Heather Sandison (34:09): Not frequent, no.
Dale Bredesen (34:11): Yeah. It’s usually when you see myoclonus especially if it’s someone who has a fairly rapid deterioration, it really makes you think about Creutzfeldt-Jakob disease, another prion disease because that’s typically has myoclonus. But there are things you might consider like valproic acid. Like Primidone, like some of the benzodiazepines, these sorts of things. I don’t know about good natural approaches to myoclonus because this is increased neural activity. But certainly, these drugs can be helpful.
Dale Bredesen (34:46): Next one here is from Luz. How can one prepare the brain for anesthesia? Please take a look. You can look either in the second book, the end of Alzheimer’s program. There’s a nice piece in there about before and after anesthesia. You can also go onto the Apollo website and look at the guides. And again, wonderful one from Julie Gregory on how to deal with anesthesia before and after. And Heather, what do you tell your patients who are going to undergo anesthesia?
Heather Sandison (35:15): Yeah. So, glutathione can be really, really helpful. Of course, work with a provider. But what we want to do is make sure that going into anesthesia, you have all the nutrients that you’re going to need to get that stuff out of you as quickly as possible. But we don’t want so much that you end up needing more and more and more of it. There’s a little bit of a balance, a tight rope we have to walk here preparing you for a surgery that requires anesthesia and then getting all those drugs out right afterwards because they can be so hard on the brain.
Heather Sandison (35:44): So, we do a couple of IVs typically before without and then a couple of IVs right after a surgery. We’d like to push the extra glutathione maybe even do some binders and just have a good detox protocol, which I’m sure it sounds like you guys have lots of resources for that and probably do something similar.
Dale Bredesen (36:01): Yeah. I think it’s a great point. And then Julia says, “I’m so happy it’s so accessible to everyone.” Fantastic, yesThank you, Heather, for making this so accessible to everyone. And then Deanna says, “How about the ketogenic diet without a gallbladder?” Now, I know Julie talks about this in the book, The First Survivors of Alzheimer’s. She has had a cholecystectomy, so no more gallbladder. She does a ketogenic diet very, very successfully. What do you tell people who have had a cholecystectomy and are concerned about going ketogenic?
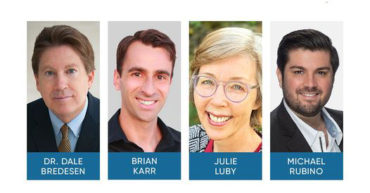
Heather Sandison (36:34): Yeah. There’s lots of strategies and I highly recommend working with the other Julie, Julie Luby. Or another health coach. Because a lot of this is a little bit of trial and error. So having smaller meals can be part of it. So not having really super high fat meals but having them more frequently instead of all at once. Taking enzymes with this, doing things, of course like TUDCA. There’s a number of supplements that can help to sort of ease this process.
Heather Sandison (37:06): If you have particular foods that you struggle with that trigger you, then working with someone to basically cut those out, but increase so that you’re not on such a restrictive diet. I love working with the health coaches, partnering with them so that you can be connecting with them regularly and getting that individualized support and the troubleshooting support. And they’ve talked to so many people about diet and the ketogenic diet in particular over the years, so they are a wealth of knowledge.
Dale Bredesen (37:36): Yeah. That’s a really good point. And then the next one here is from Christine who says, “Metabolic flexibility is key. I find older patients have variable circadian rhythm. So actually, eating every three days sometimes and resting, post feeding, since eating is energetically taxing and then a day of increased energy. So, sadly, unfortunately, these people are often medicated for restlessness. Very sad.” And certainly, metabolic flexibility, I couldn’t agree more. This is a huge issue. And again, as we’ve talked about so many times, your brain needs either some ketones or it needs some glucose.
Dale Bredesen (38:09): And unfortunately, for most of people who have cognitively declined, they’ve lost the ability to use both of those. So, they really do have an energetic emergency. So that’s why we talked earlier. You’ve got to get them insulin sensitive as well as get them into ketosis one way or another. When you look at people with their circadian, are you typically giving them two meals a day? Three meals a day? One meal a day? Or what is the typical … Or does it vary from person to person?
Heather Sandison (38:41): Yeah, so some people do really well with fasting. And especially people who have a little bit more weight or they feel overwhelmed by the thought of cooking and they’re eating to live versus like living to eat. Definitely with my patients, I individualize it. Now at Marama, because we’re in the state of California, we must feed people breakfast, lunch, and dinner. That is by law. You have to eat your dinners regularly, which is in place to protect them, which I think is totally great.
Heather Sandison (39:09): So, we do organic ketogenic, three meals a day, breakfast at eight, lunch at noon and dinner by five, so that they can get that three-hour window of fasting before going to bed, so they sleep much better as you described. And then we do two snacks in between those. Sometimes the snack is exogenous ketones. Something that will raise ketones. And what we see is that it takes about a month, sometimes six weeks for people to really settle into that.
Heather Sandison (39:40): There can be some irritability, some agitation, cravings, certainly. But once you get up over that hump and become more metabolically, flexible, become more keto adapted, there’s this nice evening out of mood and you don’t get those spikes and energy. And then the drops in energy. It’s very consistent.
Dale Bredesen (40:01): Absolutely. Next one is from Giselle who says, “Hoping for a Marama in Sao Paul, Brazil.” Yes, I couldn’t agree more Giselle. We hope that there will be access to Marama type places everywhere because they’re so needed. Absolutely.
Dale Bredesen (40:16): And then Tom says, “Is there anything to help those with vascular dementia?” I think it’s a great question because we look at what the things are … The idea here is that the major neurodegenerative conditions all represent variations on a theme of insufficiency. You have a supply; you have a demand. So, you have a neural subset. You have neural system. And so, the neuroplasticity system is what’s awry in Alzheimer’s.
Dale Bredesen (40:44): You’ve got motor control in Parkinson’s. You’ve got a combination of those in Lewy body and so forth and so on. If you adapt the protocol, we have very good results with Lewy body patients and often with vascular patients. With the Lewy body, you have to really look carefully at toxins. That seems to be a common problem and mitochondrial function.
Dale Bredesen (41:04): With the people who have vascular dementia, you really have to look at energetics, blood flow, oxygenation. Are you dropping your oxygen at night? Do you have anything, any vascular disease that’s actually preventing cerebral blood flow? Can you get the ketones up? So, it’s really more about your energetics. Do you consider things like EWOT or HBOT to get the best energetics you can? I mean, Heather, could you talk a little bit about any patients you’ve seen that has done well who has had vascular dementia.
Heather Sandison (41:39): Yeah. Exercise is what comes to mind for me first, right? Blood flow. Just delivery. Like you’re saying exactly the same thing comes to mind for me. Delivering enough resources to the brain. What we use is the contrast oxygen therapy where you alternate from a super concentrated oxygen at about 80%, air is 20%. So, you go back and forth between oxygen at 80% while you’re exercising down to oxygen around 8% or depleted oxygen.
Heather Sandison (42:12): What that does is causes vasodilation, vasoconstriction. And in that process, you basically are working the muscle of your vasculature and then increasing blood flow, blood supply. Exercise is number one. If you don’t have access to something like the LiveO2 system, just getting exercise consistently enough of it, getting your heart rate up. So, so, so important. And then as you mentioned, I would just echo all of that, getting into ketosis and working with someone to make sure that if you have stenosis, getting a cardiac calcium score, understanding what might be affecting your vasculature and getting rid of it. Is it toxins? Whatever is going on there. Getting the why. Finding the why and getting rid of it.
Dale Bredesen (42:54): That’s a great point. And then Mary is asking, “What about Medicare coverage?” And yes, coverage for this is an issue. We’re all looking. This is where the very trials that Heather was talking about a few minutes ago will help to convince Medicare that this is actually a good idea instead of waiting for people to get really sick. The average person who develops Alzheimer’s in the United States spends $350,000 by the time they pass away.
Dale Bredesen (43:20): And we had one person right in say they had
spent over a million dollars because let’s be fair, nursing homes are expensive. So, reducing the cost ahead of time can certainly help a tremendous amount. We need more trials. We need people to understand this. Now there is a group out of Sarasota, Florida called Gray Matters, and they are working to make that Medicare to cover part of the expense, and I think we’re all thinking in that direction.
Dale Bredesen (43:48): It took Dean Ornish 16 years to get the cardiovascular program covered by Medicare. So, to some extent Medicare does move slowly. Heather, how do you deal with people who come to you and say, “How can we afford to do this at Marama?”
Heather Sandison (44:05): Yeah. So Marama is actually covered by long-term care insurance.
Dale Bredesen (44:07): Oh, fantastic.
Heather Sandison (44:07): So many care residents there have long-term care insurance and they’re using it. So that does make it much more accessible. The other thing is that when you compare the cost of staying home, if you need help, oftentimes the cost of living at Marama is actually less expensive than what you would spend having a caregiver come to your home. So we hope that we are offering at good value. The issue really for us at Marama is that we don’t have space anymore.
Heather Sandison (44:38): The other thing that I want to mention here when it comes to value for your money is that I have had so many patients come to me in my office with your book and their hand and say, “I’ve gotten so much better already and I want to get to that next level, to that next edge.” And they spent $25 on your book.
Heather Sandison (44:56): What it really takes is effort, not necessarily money. The biggest impact things are exercise, sleep, and diet. And these are absolutely foundational pieces. And you can get so much just from that. So if the finances are a struggle for you, start with those things that are the lower hanging fruit, financially because they do the heaviest lifting of the entire program.
Dale Bredesen (45:21): Great. So, we’ll take the rest of these online. And Heather, thank you so much for all the great work you’re doing. And just want to remind everyone again, your upcoming summit, Reverse Alzheimer’s Summit 2.0, fantastic. From the 14th to the 21st of this month. And then you’ll have it again the next weekend. Very, very exciting. Thank you so much. We all look forward to all the experts you’ve got doing this, and let’s all work toward a world where dementia is a less onerous problem for all of us. So, we really can truly reduce the global burden of dementia. Heather, thank you so much once again.
Heather Sandison (46:00): It’s a privilege to be collaborating with you and to be part of this conversation. Thank you, Dr. Bredesen.
Dale Bredesen (46:05): Thank you. We look forward to your summit. Take care, everyone. Bye-bye.