April 9, 2021
Facebook Live: Low-Dose Naltrexone (LDN) Why it Works so Well.

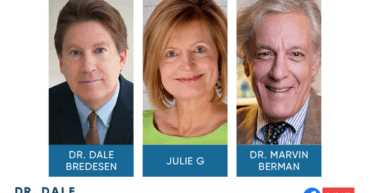
Dr. Dale Bredesen and Julie Gregory are joined by Dr. Ann Hathaway to discuss the immune system-enhancing effects of taking a low dose of naltrexone (LDN).
LDN has been prescribed to patients for quelling inflammatory conditions, and is also used in addiction recovery for its ability to increase the production of endorphins.
We’ve included a complete recording of the session and a full transcript below for your convenience.
Watch Here:
Transcript:
Dr. Bredesen: Hi everybody. Hope everyone’s doing well. I hope everyone is coming out of the pandemic and hope friends getting appropriate therapy, whatever you’ve decided for your particular situation and doing well. Really honored today to have both Dr. Ann Hathaway and Julie G with us. Welcome Ann, welcome Julie.
Dr. Hathaway: Thanks for having me.
Dr. Bredesen: Thanks for coming on.
Julie Gregory: Hi Dale.
Dr. Bredesen: We just thought it would it’d be a great opportunity here. One of the things that’s come up frequently is the use of low dose naltrexone, LDN, for a number of things. It’s been used for things like auto-immunity, for things like inflammatory conditions and of course, this was first popularized in the very famous 1985 paper from Dr. Bihari who had been working with people with addiction and found that when you use standard doses of naltrexone there were all sorts of side effects that people didn’t like. But the interesting thing was there was this remarkable rebound with you get high endorphins. And then the interesting thing is that the endorphins were so closely linked to the immune system that you get these wonderful supportive effects for the immune system. And so he used it with people who had HIV long before there was any antiviral, any triple therapy, which came out in the 1990s. So really has a very, very interesting combination. Now, when we think about things like Alzheimer’s and we think about COVID-19, as we’ve talked about before we have this unusual combination where you have the ongoing activation of the innate immune system. So you have this chronic inflammation. So to some extent, Alzheimer’s is about, you know a cytokine drizzle, just like you have a cytokine storm for COVID-19. At the same time the adaptive system is not working well enough. Whether it’s to clear herpes simplex, whether it’s to clear P.gingivalis, whether it’s to clear borrelia or bartonella, all sorts of different things that you may be exposed to. So we’re in that same situation. So we’d really like to have something that quells the inflammation but supports the immune system and especially the adaptive system. And that’s exactly the sort of thing that low dose naltrexone does. And so lots of people use it. So we’re lucky enough today, we have Dr. Hathaway who prescribes it and we have Julie G who’s had some wonderful experience with it. So maybe Ann, if we start with you I know you’ve been using this for your patients and tell us how you decide what patients to prescribe this for.
Dr. Hathaway: Yeah, it’s a very interesting substance because it falls into this category where it has a very different response. People probably are aware of naltrexone itself at 50 milligram or a 100 milligram doses as something that reverses an opiate, a heroin or an opiate overdose. Or people take it as a kind of a way to stop themselves from their addiction to opiates. But we have something called a hormetic response with a low dose which means it has a very different reaction in the body. So when you block the opiate receptors, of course, you’re going to get increased pain. When you take a low dose, you’re going to get what turns out to be a decrease in pain and inflammation in the body. So there are a very, very broad range of instances where low dose naltrexone could be effective. I’ve used it in many, many types of auto-immune diseases. Certainly I have lots and lots of patients with autoimmune thyroiditis and almost all of them would be on low dose naltrexone. And it is important to be aware of possible issues with low dose naltrexone and it’s good to start with a very low dose somewhere between 0.5 milligrams in a very sensitive patient to a more usual 1-1.5 milligrams, and then build up to a dose of either usually three to 4.5 milligrams is a, the treating dose that we use. So I’ve used it in many post-cancer patients. I’ve used it in people with all different types of chronic pain, chronic headaches, chronic backaches. It can make a big difference. And we also use it in cancer because it boosts your immune system in such a way that you have, your own immune system is better able to fight off the cancer cells. So those are some of the situations where I’ve used low dose naltrexone. And for the most part it’s been very, very effective.
Dr. Bredesen: Yeah. And certainly neuroinflammation is something we hear about all the time. Neuroinflammation is important in Alzheimer’s and pre-Alzheimer’s. It’s important in Parkinson’s disease. It’s important in Lewy body disease. It’s important in frontotemporal dementia and you can just go right down the list. So neuroinflammation comes up again and again and again. And so therefore, you know, it’s a very reasonable approach and I know some of your patients who have cognitive decline, that you’re treating for cognitive decline you are including LDN. Is that fair to say?
Dr. Hathaway: Absolutely. Yeah. We know that in Alzheimer’s disease and all neurogenerative diseases we have increased activation of the microglia, the immune cells in the brain. And those cells become overactive in all neurodegenerative diseases. So it makes perfect sense to me that adding low dose naltrexone to, of course what would be an overall strategy to address all the various factors in pre-Alzheimer’s or Alzheimer’s disease, it would certainly make sense to add low dose naltrexone. And it has been a part of many of my patient’s regimen to try them on low dose naltrexone.
Dr. Bredesen: Yeah. Good point. And certainly, you know, as you mentioned the hormetic effect, so this rebound, this nice rebound effect, and, you know, if you look at this and essentially exercise is low dose muscle damage. And so, you know, you’re responding to that exercise by making more muscle you’re improving. So to some extent low dose naltrexone is exercise for your immune system. And Julie, I know that you have been prescribed this before by your physician. And tell us a little bit, if you would about your experience with this.
Julie Gregory: Sure. You know, I have to say that of all the different supplements and things that I take this is probably the one thing that I would not want to be without. You know, when you’re taking Omega-3’s, you know you’re boosting your Omega-3 index but you don’t really feel any differently. I feel very differently when I take LDN. I feel very relaxed. I feel very peaceful. I have a tremendous amount of energy. I sleep really well. I mean, there was a very noticeable difference before I took it and after I started taking it. And I had some very important objective indications of improvements in my health. So I have an immune deficiency. I have low IgG. And my IgG, the first month I began taking it, boosted up by a hundred points.
Dr. Bredesen: Wow.
Julie Gregory: I also have subclinical hypothyroidism and I was able to cut my medication in half, like within two days I actually became hyperthyroid, which is one of the things that you’re told to look out for. So within several days of starting, just at 1.5 milligrams I began to get some tachycardia and I couldn’t figure out what was going on. And then I remembered what my physician said that if I begin to get any symptoms of an overly active thyroid to immediately cut my medication and I’ve been able to sustain that improvement. So I think it’s one of the most important supplements or medications that I am taking.
Dr. Bredesen: Absolutely. And talk a little bit about when you take it, just because, you know the effect then lasts through days. And in fact, people who’ve been on it for a while and the guy who invented it, actually took it for 10 years himself. One of the big advantages of this approach is that there’ve been very, very few side effects as long as you’re not too high of a dose.
Julie Gregory: Right. So I take it in the evening, and I try to take it as late as possible which is hard for me because I go to bed pretty early.
Dr. Bredesen: Yeah.
Julie Gregory: I notice it if I take it too early, I tend to wake up too early. Because once your body begins to get flooded with those endorphins, you are ready to take on the day. I used to need a cup or two of coffee in the morning. Now coffee’s nice, but I certainly don’t need it. I mean, I wake up with a tremendous amount of focus and energy and I’m just really happy, peaceful and calm. I mean, I really, really think this is so beneficial. I think, especially for ApoE4 carriers because we’re often described as carrying the pro-inflammatory allele. And in a lot of your talks, you describe the immune systems of ApoE4 carriers us as being almost militant, you know, like soldiers at the ready. Our immune system is hyper-responsive, ready to take on whatever is thrown our way; whereas people who carry the other APOE genotypes are very relaxed. You portray them as living in a hippie commune, full of peace and love. I feel like when I began taking LDN, I joined the other side.
Dr. Bredesen: Good.
Julie Gregory: In that, I mean that it’s been amazing.
Dr. Bredesen: Interesting, yeah. And of course people would use it for multiple sclerosis as an example. And you think there are some very interesting relationships between MS and Alzheimer’s. So with MS there’s a large inflammatory component, and auto-immune component, but there’s also a smaller degenerative component, unfortunately. And so people with MS tend to have some degeneration over the years. With Alzheimer’s it’s the other way around. You do have some inflammatory component, but you have the degenerative component, which is the predominant one, but there are many parallels. And so it’s been used successfully with MS and people are looking at, okay, should this be used more with people who have cognitive decline. Now, unfortunately an early trial back in the 1980s used whopping doses of a 100 milligrams and no surprise saw no improvement. But smaller doses, this thing, you know, the typical LDN of three milligrams per day or so, you know really looks much, much more promising. So, Ann could you talk about people, side effects that people. You mentioned that the issue of, you know, kind of at times sleeplessness that this can be a problem if people start out too high. You mentioned starting nice and low and then working up. Do you typically try to end up with somewhere around 3mg or so?
Dr. Hathaway: Somewhere between 3 and 4.5 mg. I would say a lot of my patients are on 3 and maybe at least 50% of them are up to 4 or 4.5 as their optimal dose. I, you know, I talk with them about trying to think about the benefits versus side effects and figuring out where they are. Some of the side effects. First of all, one of the positive side effects is mood improvement which Julie talked about at length. It’s been interesting. I’ve had several young women with hypothyroidism with autoimmune hypothyroidism, who on their dose stopped their anxiety eating and felt and went to a normal weight. So obviously it’s, you know, part of the opiate increased reaction is an increase in endorphins. And that’s a big piece that’s going on here when we’re decreasing neuroinflammation. But some of the side effects that I warn people about are sleep disturbances. Some people get very vivid dreams.
Dr. Bredesen: Yeah.
Dr. Hathaway: And if someone has a tendency to have already scary dreams or very vivid dreams, then you want to be very cautious about that and start them maybe on a really tiny dose like a 0.3 or so and work up really gradually to see if they tolerate it. So that’s really the big thing that I worry about with. I have had one or two patients who had got overamped, just feeling really kind of hyper and a rapid heart rate, for example. And there was, I have had a couple people who just didn’t tolerate it at any dose. So it’s not for every single person. You have to you know, you have to really be careful with your patients and listen to what they’re saying and if they’re not tolerating it. One thing you can do with someone who has a real issue with the high drama dreams or too scary dreams is you can give it in the morning. It doesn’t have to absolutely have to be taken at night although it is recommended if possible to take it before bedtime.
Dr. Bredesen: Yeah, that’s a great point. Okay, so there are lots of good questions here. Let’s go through some of these. Priya asks has it been used in autism to help with viral encephalitis? This is a really interesting point. Certainly, you know antiviral effects because of the immune support one of the reasons that people have been interested. And one of the concerns that Dr. Bihari had when he first was using this, he said, he’s worried that people will think it’s snake oil because it seems to be helpful for many things. They found people could actually reject to their lymphomas in some cases. They found that HIV patients had fewer opportunistic infections, fewer cancers, did better overall. They found that people had less pain. You mentioned the mood effects. Less inflammation, less auto-immunity. So he said, you know, it begins to sound like snake oil, and we hear something like that, of course, the question always comes up is this part of what we’re simply experiencing because of our age and because of our lifestyle? Maybe that’s why this seems to be so good. Maybe many of us have sub-optimal immune systems and that’s certainly not out of the question. So for certainly, if there’s a question about viral encephalitis, it may, again as with, just as occurred with HIV it’s very helpful to have an antiviral as well but of supporting the immune system would be great. Now, obviously there are many people who have autism who don’t have viral encephalitis that can have all sorts of other things from genetic changes to various toxins they’re exposed to, to, you know, to idiopathic, we don’t know. But certainly it could potentially be helpful. And again, we recommend please talk to your physician. This is the critical piece. Ann, have you ever used it for people who had autism spectrum disorders?
Dr. Hathaway: Certainly, it makes sense that in autism spectrum there is some degree of neuroinflammation so from that point of view it makes sense to me. I certainly have had people on the spectrum in my practice and some of them have been on low dose naltrexone. But I haven’t been treating severe autism in my practice for quite a while, but that those patients tend to go to someone who absolutely specializes in that field. But in the case of autism spectrum disorder people who are fairly, fairly functional I have seen LDN be helpful for some of the issues that can go along with autism spectrum, like anxiety and depression.
Dr. Bredesen: Yeah, yeah. That’s a good point. And I think, you know we’re hearing from the autism community, the same sorts of things that we are seeing with Alzheimer’s disease that there are multiple factors, that the gut is involved in many people, that there are toxins involved, there are infections and inflammation involved, as you said. So I think, you know, we’re coming away with the repeated suggestion that this is a multifactorial disease which are not even disease. I say multifactorial problem with a spectrum just as we see with cognitive changes. The next one here, Susan says I take 4.5mg daily prescribed by my functional doctor. Yeah, so you’re right in line with what Ann was just talking about. That’s a good point. And hopefully it’s helping you. Kim says, what about auto-immune? Absolutely. This is the area where it was recommended probably most. And again, things like, things that we think of as auto-immune diseases from lupus to rheumatoid arthritis to multiple sclerosis and things like that. And you mentioned, Kim mentioned much lower doses, 0.5 to 1.0mg, and Ann you just mentioned the same thing to certainly start low. The reason that slightly higher doses were used was Dr. Bihari when he was first using this they actually did careful studies going all the way down and starting at a 100mg and then going lower and lower and lower and seeing where you get this nice rebound which is what he was looking for with the endorphin increase. And what he found is that that cut out when you got below three. So you were down at half or one, you weren’t getting that nice response. Now in some people you still do. So that’s why, again, you have to adjust it and Julie, maybe you could talk for a minute about the fact that you ended up adjusting your own and ended up where you are currently.
Julie Gregory: Right. I started at 1.5mg. And I have to say that on the first day I felt really out of it. I mean, it’s not like it was immediately helpful but I believed in the benefit enough to stick with it. And then by the second day I was getting the weird heart rate, but I was warned about that. So I continued at the 1.5 and cut the thyroid medication. And then after a week or so I went up to 3.0mg and that was pretty amazing. I then went up to 4.5mg and at 4.5mg I think I mentioned that I felt too energetic in the morning and then exhausted by the afternoon. So I learned my sweet spot was 3mg, yeah.
Dr. Bredesen: Yeah, great. Okay and then here Maria says I’ve used only in ICU as Narcan so fascinating. Erythema multiforme, my doctors have been trying everything to help flare ups and reduce inflammation. So, yeah and when that flares up, the dementia symptoms are awful. Yeah, very good point. So this comes back I think you make a really good point, Maria. This comes back to the fact and we see it again and again. Anything that is driving this inflammation and it’s often systemic, but it can also be as Ann said, the microglia in your brain. These things will increase problems with cognition. There’s just no question and we see it again and again, and again. People who will be improving for example on the protocol will suddenly have a viral illness or they’ll suddenly have some stressor, you know one of these things and no question, they take a step back and then they kind of have to work their way up again. So inflammation ongoing this is a problem because you have to remember the amyloid beta that we associate with Alzheimer’s disease is a part of your innate immune system. So when you’re pouring this stuff out, you are pouring out a beta as well. And so no questions to be able to decrease that and of course we want to get at what’s causing that inflammation, but in your case, as you say when you get your flares, yeah maybe you should talk to your doctor about the possibility of his or her recommending LDN. And then Wendy asks, how long should you stay on 3mg? Is a great point. You’re on for EBV. One of the points that Dr. Bihari made is that there were people on it for 12 and 14 years without any problem. And of course at the time he was seeing wonderful results with people with HIV. This was in the pre-triple therapy era. So this has been one of the exciting things about it. There don’t, there do not seem to be long term negative side effects. So let me ask you Ann, are there people where you say, okay enough now it’s time to start backing off this? And if so, how do you decide.
Dr. Hathaway: I have not had that experience. I have had many people who, you know, as things go in a clinical practice, people kind of drift away for, they’re feeling better and you don’t see them for a year or two. And then you hear back from them like, hey I’m not doing so well. Let’s meet. And one of the things that often has gone. Because LDN, low dose LDN is a prescription item. So with prescription items, you need to see the person and check in with them every year or you’re not going to refill them, right. So that’s one of the things that sometimes people notice, Oh my gosh, I’m not taking my LDN anymore. I ran out. I just kind of was busy and forgot about it and now I’m not doing as well. So I’ve had that experience rather than people on LDN saying, you know. Sometimes people for cost, you know, it’s not an expensive medication but for some people, cost is budgets are tight, right? So they might say, I’m going try going off it. And I say, sure, absolutely. And occasionally those people stay off it and they don’t notice too much. So that does happen. But more often people will come back and say you know, I really do think I would like to refill my low dose naltrexone. I think it was helping me.
Dr. Hathaway: So-
Dr. Bredesen: And when you do that people come off do you recommend that they come off very slowly?
Dr. Hathaway: I would recommend that, but honestly, most of the time people go off on their own.
Dr. Bredesen: I see.
Dr. Hathaway: And I haven’t heard from them like, oh my gosh, I had side effects of going off.
Dr. Bredesen: Okay, good point.
Julie Gregory: Thank you guys. I just want to mention something. I joined a few of the LDN support groups. And some people, if LDN is no longer is giving them the amazing initial effect that it did, some people take a holiday. They stop taking it for a day or two and then resume. And once again, they’re getting amazing benefits. So that is something to consider. I’ve seen people cycle it.
Dr. Bredesen: This is a really good point. Yeah, because anything where you’re pushing to be able to kind of get a little holiday off of them and get back on, will give you better effect. So that’s a really good point. The next one here is from Gail. Gail asks would you prescribe low dose naltrexone for prevention? And I think you really hit the nail on the head, Gail. So thank you for asking that question. This is something we talk about all the time. Do we want to suggest people get into ketosis, for example? How much do you want to do for prevention? Well, you know, remember that if you’re going start having symptoms, you know that that can be a big problem. And so we want to do as much as possible at the same time, you don’t have to do as much. Thankfully you don’t have to do as much for prevention as you need to for reversal. And again, the longer you wait the more you have to do. So we’d like to get as many people as possible on prevention or the very earliest reversal with initial symptoms. So, great question. You know, so let me ask you Ann, for people who come to see you who are there for prevention, I know you have a number of patients who are seeing you for prevention. Would you consider something like this or are there certain, is there a certain metabolic profile that would suggest to you that this would be part of the armamentarium? Or would you always wait until there are symptoms?
Dr. Hathaway: I think it makes sense thinking about it that if someone is higher risk in any way, carrier of an ApoE4, chronic inflammation of other kinds, etc., I think it makes sense. Again, because low dose naltrexone is so benign in almost every case, you know, I don’t see any reason why we wouldn’t consider it for prevention, you know especially for ApoE4 carriers, for example or someone who has autoimmune disease or someone who has chronic pain, you know. It’s of course been shown in research to be extremely effective for fibromyalgia, which is a type of pain that is considered to be centrally initiated. It has a central cause rather than, you know if you have knee arthritis and you have knee pain. Of course, that does create inflammation in your entire body, but fibromyalgia is a more specific neuroinflammatory kind of problem.
Dr. Bredesen: Yeah.
Dr. Hathaway: Right, so I would, I would definitely consider low dose naltrexone for prevention, yes.
Dr. Bredesen: It’s a good point. And you know, one thing we could think about is we have people who will have a clear part of this is from inflammation so especially the type one, the inflammatory people. If you have a high risk for this maybe you are still there for prevention, but you’ve already got a high hs-CRP or you’ve got inflammatory component, that would be one you might think about more. And then the other thing is we do see people where they have all sorts of auto antibodies. When you start looking at auto antibody panels they just light up across the board. And I tend to think of that as kind of the next step because there, it’s not necessarily that their innate immune system is activated but now their adaptive system is activated but unfortunately it’s not focused on the pathogens. It’s broad enough that you’ve now got all these different auto antibodies and that’s another group where they might do very, very well. Whereas people who have a very good immune system and have no auto antibodies and no ongoing inflammation, they may not get as much out of it. And I know Julie, to some extent, you know you’re obviously in a prevention mode having done all the wonderful things you’ve done in the past. And I guess the question there would be, you’re obviously in a good situation with your immune system but you did, you know, you don’t have a high hs-CRP, you don’t have ongoing inflammatory markers. But as you mentioned, the ApoE4 itself is a pro-inflammatory protein. And so certainly you’d have one good reason, you know one good reason to think about it. And as you pointed out, maybe anyone with a ApoE4 who’s going have a more pro-inflammatory response to things which something that is as Professor Finch has taught all of us probably helped in the primordial hominids five, you know five to seven million years ago. So what would for Julie, for you, what would tell you, hey, I don’t think I need this anymore?
Julie Gregory: I guess I would probably have to go off of it and see if I felt any differently.
Dr. Bredesen: Yeah.
Julie Gregory: And I would say for a sustained period of time, like go off it for a week to see if I feel any differently.
Dr. Bredesen: Yeah.
Julie Gregory: I really don’t have any desire to do that because the benefits been so great. And while my standard inflammatory markers have all been low, I have been diagnosed with CIRS. So, I have had some other inflammatory biomarkers that have been sky high at times and they’re all going down now since I’ve treated the …
Dr. Bredesen: Great.
Julie Gregory: The babesiosis. But my TGF beta1 and C4A have been very elevated. So I think for the type 3s this is an amazing, you know, opportunity to use it.
Dr. Bredesen: Yeah, and as they say, you know CIRS is chronic inflammatory response syndrome, dampening down that inflammation
Julie Gregory: Right.
Dr. Bredesen: Good to get rid of what’s causing it but also good to get rid of the response itself.
Julie Gregory: Right.
Dr. Bredesen: So, and Leo asks a very relevant question here. What about polyneuropathy pain? And of course, peripheral neuropathy is something very common, many, many different causes much like these other degenerative changes. So, this is a peripheral neuropathy, and you can have it from changes in nutrition, you can have it from ongoing inflammation, you can have it from various infections, toxins on and on. And so, Ann have you ever used this for peripheral neuropathy patients?
Dr. Hathaway: I don’t think so. I have seen, you know, a number of over the years, chronic inflammatory people who have also peripheral neuropathy. And it makes sense to me that would be a good idea. One of the things that has occurred to me in kind of preparing for this, for this Facebook live is how many opportunities there are with our patients to use low dose naltrexone. And I think that one of the effects for me of doing this Facebook live in preparation for it is that I’m going be thinking about using low dose naltrexone quite a bit more and hopefully learn a lot more about it.
Dr. Bredesen: Great point. And then Marta says I’m on, just to finish up with Leo. So absolutely it’s used for chronic pain for many people. So certainly something, please, please consider talking to your doctor about it. Marta says I’m on 4.5mg, but no difference after months of taking it. So difference in what? So the question is what were you taking it for and what’s happened. So, and then maybe you need to actually go to a slightly lower dose. I don’t know, but certainly it would be helpful to know when you say no difference in what. And then Rajia says, this is interesting with MS I was told I shouldn’t take it because it boosts immune function. It’s confusing, yes. You know, and you bring up such a good point. This is something that is interesting that there, this is, it’s almost as if it’s an adaptogen for the immune system. It seems to suppress the innate part, the inflammatory part. It seems to suppress the auto-immunity in some sense because as was pointed out initially when it was first used it seems to sharpen the response so that you’re getting a response of the immune system to the problem, to the pathogen or whatever it’s responding to and you’re not getting this broadened response to other things. So that you’re getting rid of the auto antibodies and you’re now focusing on a very, a very specific immune response. So, in fact, it has been used for MS and you may want to talk to some other MS experts about this especially ones who have a history of using this. So you might consider it. You’re right, that theoretically the fact that it supports the immune system could give you problems but the experienced so far has been that it seems to be helpful instead of harmful for MS.
Dr. Hathaway: Yeah. I’ve seen blood brain barrier auto antibodies go down as well as myasthenia gravis markers in ocular myasthenia. And certainly in many Hashimoto’s patients, their autoimmune markers drop. So I’ve seen, you know, we are looking for the of course the clinical benefits, the person to feel better in various ways. But also we do see objective benefits in terms of the clinical markers.
Dr. Bredesen: Okay, then we’ll see the next one here. Let’s see, okay. So Michael saying, wow, Julie, the benefits of LDN for you are quite impressive. Thank you for sharing. Is there a doctor’s prescription needed to use LDN? And yes, there is. This is the medication.
Julie Gregory: Yes. You mentioned that you probably can’t go to your family physician and ask for this. Yeah, you need to work with a functional medicine physician you know, or someone like that, an integrative physician. Ann, what do you think?
Dr. Hathaway: So, there is an organization called the LDN Research Trust and they have listed there almost every piece of scientific research related to low dose naltrexone, which is a nice research to have, but they also have a link to hook you up with a physician who has skill and experience using low dose naltrexone if you want to specifically focus on that. I think almost every functional medicine doctor would be familiar with low dose naltrexone, but there might be some new to functional medicine who are not. So, but that is a great resource, LDN Research Trust.
Dr. Bredesen: Yeah. So yeah, these are all really good questions. And then Marta says, let’s see here. Sorry, Regina says, be careful near 4.5 for breathing issues. And Ann, have you had any patients who had any breathing issues with this dose?
Dr. Hathaway: I have not, no. Which is not to say it could not occur, but I have not. I, as I said, I had one patient who even on a 0.5 dose had an increase in her heart rate and just, you know, just did not tolerate it. So it’s, you know, you do have to work with the physician and be careful with it. And you want to work with someone who has experience with it, not just ask your, not just beg your family doctor to prescribe it for you.
Julie Gregory: They’re not going know what you’re talking about, I promise.
Dr. Hathaway: Right, right.
Dr. Bredesen: And then let’s see here, Andrea says I’m extremely disappointed that you’re endorsing LDN. I’ve seen it increase Hashimoto’s antibodies. And so in Julie, you address this issue of increased heart rate, which would be typically the opposite of this, but she says, test and retest. This is not root cause medicine. So Andrea, I’m really glad you brought this up. This is such an important point. Absolutely. You know, as someone, you know, both Ann and I were trained in very classical medicine, prescription pad medicine. We both came to the conclusion through years of seeing patients and doing research that we need to do root cause medicine. That is the future to understand, as we say 20th century medicine was about what it is. 21st century medicine is about why it is. And we are very interested in systems biology and how these things all work together. No question. But please remember also, when we see people with cognitive decline, one of two things is going happen. Either we’re going help them or they’re going to die. So this is a horrible terminal illness, cognitive decline, ending up with Alzheimer’s. And so we, and we do see people where they’ll get into a plateau and the question is, how can we improve them? How can we keep them from having problems in the future? And so one of the questions is can we improve their immune system? Because that does seem to be one of the rate limiting problems. We see again and again and again, there will be a rate limiting problem for somebody. Either they won’t get into ketosis or they’ll have an ongoing exposure to mycotoxins. They, you know, they won’t want to move out of that house with all the mycotoxins or they’ll have, you know an infection that hasn’t been identified maybe bartonella or babesia. So you’re absolutely right. We’re trying to do the best we can with root cause medicine but we’re also asking, is there anything we can do? We got to pull out all the stops for people who are otherwise dying from cognitive decline which ends up as in many cases, as Alzheimer’s disease. So you make a very good point, but please remember we have a lot of people out there, about 45 million of the currently living Americans will die of Alzheimer’s if we don’t do our best for prevention and reversal. But, you know, your point’s well taken. You know please check and recheck to make sure that you’re getting a beneficial effect. And this is why, as we’ve said before, it’s that follow up. This is where Julie has done such a great job with each thing she does she then does quick follow-up. Okay, how am I doing? Are things better? Subjectively, objectively? You know, what’s happened to my IgG? What’s happened to my cognition? What’s happened to my energy? And I think, you know, that is what’s helping to get that feedback because it’s true. The same thing is not the best for everybody. This is personalized precision medicine. It is different for each person. Marianne says, would it help with chronic Lyme? And Julie, I know you’ve been to Dr. Schweig, who’s the expert on Lyme disease and so maybe you can speak to that point.
Julie Gregory: My guess is absolutely because chronic Lyme is chronic inflammation, right? Widespread inflammation. So I had chronic babesiosis for probably 15 years that led to my type 3 diagnosis, to my CIRS. And it’s been very helpful for me. So I would think it also be very helpful for chronic Lyme.
Dr. Bredesen: Yeah, great point. All right. And then let’s see, Kofi asks, is it any good for atrial fibrillation? I guess my, theoretically my big concern would be if you now see an increase in thyroid activity you’re going have more problem with atrial fibrillation. So I’d be, you know very careful. And again, talk to your doctor extensively about this if you have atrial fibrillation. Ann do any of your patients who are taking LDN, do any of them have atrial fibrillation?
Dr. Hathaway: I would be very cautious in a situation with atrial fibrillation. Certainly we worry about that if we increase thyroid doses. We worry about that in anything that’s going to provide more stimulation, more adrenaline, more anything that’s a stimulant to the body. So, I wouldn’t say, you know, absolutely never someone who has a chronic intermittent atrial fib might still be all right as a candidate for low dose naltrexone, but it would be with extreme caution.
Dr. Bredesen: Yeah. And then Kim asks another question which is here about LDN and other medications. Ann are you concerned about interactions? We’ve already talked about the thyroid issue, obviously the Julie pointed out. Are there other medications that you’re concerned about in terms of interactions with LDN?
Dr. Hathaway: I have not seen it have significant interactions with other medications. The vast majority of my patients are not on a lot of medications. Certainly I would not be concerned about it with Aricept or Namenda. I don’t think there’s a conflict there. I generally don’t start patients on those medications but of course, some patients come to me already on those medications and I would not consider those a contraindication to low dose naltrexone. Yeah, antidepressants. It seems to be fine with antidepressants. Certainly I have some patients who take antidepressants. Yeah, I can’t think of …
Julie Gregory: Yeah.
Dr. Hathaway: You know strong problems there.
Dr. Bredesen: Yeah.
Julie Gregory: I can think of one. If you were to be in an accident and you were to need pain medication, you’d have a period of time where the pain medication might not be as effective as it otherwise would be. And I just know this because I had a ski accident, pretty close to when I’d started it and I opted to continue with the LDN and not to take any pain medication even though I had a broken rib and a concussion because the benefit was so good from the LDN. And so yeah, I mean that’s something that I know some people are sort of on the lookout for, but I think that suppression of pain medication would only be for the three or four hours that you’re right after you take your dosage. So it’s a relatively short-lived period.
Dr. Bredesen: But also remember Julie, since you’re getting, what’s happening with this as each day your endogenous endorphins are higher because of this.
Julie Gregory: Absolutely true.
Dr. Bredesen: So, it wasn’t quite as bad as it might have been. All right, and then Karen says, my doctor has suggested I try this because I tend to convert T4 to reverse T3 instead of free T3. And certainly, you know this is something that you see a lot with people especially who are under chronic stress. You tend to convert more to the reverse T3 and it’s a concern. So that it’s interesting. It’s something to consider. And Ann, have you seen changes in terms of conversion reverse T3 versus free T3 in people on LDN?
Dr. Hathaway: Certainly, I’ve seen quite a few people drop their reverse T3 with multiple different types of functional medicine interventions. But yeah, I think I have seen low dose naltrexone as an alteration drop the reverse T3 and in a few cases. Yeah, I think that’s a reasonable thought.
Dr. Bredesen: And Melissa says many people with fibromyalgia do well with LDN and great point. Ann you talked about this before. This is very good point and it’s certainly something to consider. Debra says important to know that it can also solve sleep troubles. Helped a patient of mine get off THC which I didn’t like seeing her take the sleep and improve her mood as you notice. Yeah, very good point. And you know, we hear so much about CBD oil as well lately and, you know should we be thinking instead of CBD oil for sleep, should we be thinking more on the LDN side for sleep? So, and, okay, so let’s go to the next question here. Let’s see. This is, is useful for things like. So Barbara asks, might this be useful for depression? And of course there’s a lot written about depression and inflammation over the last few years. So I think it’s going to depend a little bit. I’m not, to be fair I’m not a psychiatrist. And so I, you know you might want to talk to a psychiatrist who is a functional psychiatrist who would be using this. But certainly for those people who have depression associated with a leaky gut and inflammation might be something to, again to talk to a functional psychiatrist about. Certainly as you mentioned it seems to have positive effects on mood for many, many people. Let’s see here. Let’s do one here. Let’s see Karen saying the doctor’s recommended to keep the reverse T3 in check as we talked about a minute ago. Right now I take a bit lower dose plus extra T3 instead of. Would LDN help with this? Okay, great point. So, you know, again, I would talk to your physician. You’re going, obviously this is a situation where you’re going have to kind of titrate things to get the best results. And let’s see, Maria is asking what blood tests would you recommend prior to taking this? So Ann, what do you recommend for your patients prior to starting them on LDN?
Dr. Hathaway: Well, you know, I do a lot of testing. I like to, as we say, cast a wide net, right? So when I see a new patient, I do, you know, what most physicians would consider a massive amount of testing.
Dr. Bredesen: Yeah.
Dr. Hathaway: And that’s always going include some inflammatory markers, at least CRP and SED rate, if not, you know, IL-6, IL-2 in certain cases, right? So those would be any hint of autoimmune disease, If you want to get an ANA. There’s certain people who carry a high positive ANA but they have no diagnosed autoimmune illness. So that’s good to know as kind of a marker. Certainly thyroid antibodies, all these kinds of things are things you might look for a shift in, an improvement in after you have initiated and got them on their optimal dose of low dose naltrexone. So, those are some things to consider if you get, if you have someone with cognitive decline and you want to go ahead with more you might do certain kinds of panels that look at blood-brain barrier antibodies or anti-tubulin antibodies, things like that that look more closely at antibodies that might be involved in neurodegenerative processes. So those are some of the things you might want to look at and then look for improvement in them on low dose naltrexone.
Dr. Bredesen Yeah and certainly it’s been shown to reduce inflammatory cytokines. So for people who have high IL-1, IL-6, TNF-alpha for all those things. And then I wonder about the various things that Dr. Shoemaker has recommended. Things like C4A and TGF beta1. these could potentially be impacted by this as well, which again, brings us back to the fact that it’s a very relevant for some of the things that are driving cognitive decline in so many people. So, all right, well, let’s end there and let’s take the rest of the questions online. Thanks for some absolutely outstanding questions everyone. Thank you so much Ann for your expert discussion. Thank you, Julie for your discussion, with all your background and your use of this. I think this has been very, very helpful. And thanks to everyone. Please stay safe as we’re coming out of this pandemic and I hope that everyone is doing well. Happy spring to everybody.
Dr. Hathaway: All right. Thanks Dale. Thanks Julie.
Dr. Bredesen: Thanks everybody.