May 13, 2021
Facebook Live: A Family Affair

Watch here:
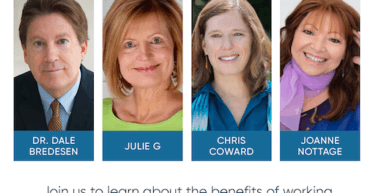
In this Facebook Live, Apollo Health’s Chief Science Officer, Dr. Dale Bredesen, and Chief Health Liaison Julie Gregory were joined by Julie G’s husband Bruce Gregory, ReCODE Certified Coach Julie Luby, and VP of Coaching, Chris Coward for an insider’s look at living and practicing the Bredesen Protocol® within the context of family dynamics. The Bredesen Protocol is a multifactorial, personalized precision medicine approach exclusively offered through the ReCODE and PreCODE programs.
We’ve included a complete recording of the session and a full transcript below for your convenience.
Watch here:
Transcript:
Dr. Bredesen: Hi everybody, great to have you with us. We’re so fortunate today, we just have a fantastic group here. So Julie is always with me on these Facebook Lives. And today she is with her husband Bruce. Welcome Julie, welcome Bruce.
Julie Gregory: Hey there.
Bruce Gregory: Hello.
Dr. Bredesen: And we’re also very fortunate to have Christine Coward who is a wonderful health coach. And also Julie Luby, a health coach. And they both have their own family stories related to cognitive changed. And so we thought it would be a really good idea. One of the things that isn’t talked about enough is the interdependence. How critical it is the interaction between people who are either experiencing cognitive decline or who are at high risk for cognitive decline and other family members. Who can range from you know they’re not involved, or they’re heavily involved, or they’re negatively involved? Or they’re positively involved. And what happens is, and there’s a relatively large literature on this that both on the side of the caregivers, the caregivers actually tend to develop diseases that are associated with stress early. They have shortened telomeres for example. And so in fact it actually hurts the caregivers. And on the other hand, of course what the caregiver does is critical for the outcome of the patient or the person at risk. So we thought it would be a great idea, Julie’s just done so extremely well for over nine years now. And interestingly far from impacting Bruce in a negative way as you’re going to hear, it’s impacted Bruce in a positive way for his own health and his own life. So it’s just been a fantastic model. But I want to go back Bruce if we could for a minute to way back when Julie was first finding out, when she was having her own cognitive issues. You are a pilot for a major airline and so you’re getting there, you are responsible for the lives of hundreds and hundreds of people all the time. So you’ve got to focus on that. And at the same time you’re being told by your wife that she’s got the highest genetic risk and she’s having her own cognitive issues. So how did you keep it together at that time? What went through your mind when your relatively young wife in her late 40’s at that time was dealing with what could be a terminal illness?
Bruce Gregory: Well, it was very stressful. Being a pilot you try to get everything taken care of before you’re going on a trip. You try to get all the loose ends tied up and everything good. But then when you’re gone you’re thinking that your wife is not being able to do everything on her own, things are falling apart at home. And you’re not there to pick up the slack or whatever. And then that kind of weighs extremely heavy on your mind. And I have to admit, I wasn’t truly a “caregiver”. Because Julie was extremely strong, very tenacious and fought extremely hard to find answers, to find out what would work, to find an avenue. She’s a fighter and she’s, well between her and I, she’s way brighter than I. So, she did a lot of research.
Dr. Bredesen: That’s true for all of us with her.
Bruce Gregory: And I’m very fortunate in that regard. But I kind of like hung on her shirttail following the protocol. Because she was under one diet, one protocol and if I did something else, I wouldn’t like having two different religions in the same house, you’re celebrating a different holiday. And to be of one mind and support each other, it just worked so much better. But it was quite a few changes and a lot of scary moments especially in the beginning because everything was new territory. Everything was kind of untested. And every time you went to something traditional, traditional medical advice, it wasn’t very good. I mean in all reality if we followed traditional medical advice, Julie would be dead, I’d be about 250 pounds, and I’d probably be ending my airline career right now just for medical reasons.
Dr. Bredesen: I wish I could say that’s exaggeration, but I think what you said is probably true.
Bruce Gregory: Yeah, and it was a lot of work, a lot of mindset changes and fighting a lot of childhood mindsets that I grew up with. And so it’s like reinventing everything that was told since you were a kid and saying it’s not right and changing it. So that was hard, that was hard. And then also to take those ideas, those changes and implement them when you travel on the road. That’s an art in itself.
Dr. Bredesen: Right. And then of course with the experts telling you to just get on the medication, that’s got to be tough. So was there a moment when you kind of shifted from wait a minute my wife has what I’m being told is a terminal illness to wait a minute maybe she’s going to fight her way through and actually survive this and maybe even thrive on this. Was there a time when you kind of saw that change or did you just never doubt from the beginning that she was going to find a way to fool all the doctors?
Bruce Gregory: I never thought she was going to fool all the doctors in the beginning, I really didn’t.
Julie Gregory: No, it was scary.
Bruce Gregory: Because it was scary, it was kind of a dark thing. And then we went from doctor to doctor to doctor and got negative answers all the time. But when I’d go into the study late at night and there’s Julie banging away at the computer and it was the internet that kind of saved her. Just being able to connect and find out who’s doing the latest research. And her tenacity and her drive is really what changed everything. And then seeing her have these breakthrough aha moments where she would make a connection with a research physician or whatever. I almost remember where we were at each one of these aha moments she would have in her discoveries. I mean they were very pivotal.
Julie Gregory: Yeah, we should remind people that this was nine years. And your pivotal paper hadn’t been published yet. I didn’t know of you. And at that time we were told Alzheimer’s can’t be prevented, it’s untreatable and it’s incurable. It’s progressive and most people are dead within 10 years. So given that I was already experiencing symptoms, it was a really scary time. And I did search very hard for answers. And slowly over time we found them.
Dr. Bredesen: You were burning the candle at both ends on your job.
Julie Gregory: Well, I couldn’t have been successful if Bruce hadn’t had implemented the changes with me.
Dr. Bredesen: I think that’s a critical piece.
Bruce Gregory: It didn’t take long to realize that that was really the most selfish thing I could do was implement these changes. I got one quick thing I got to add. You know, just before we started this protocol, the summer before I rode 4,000 miles on my bicycle because I knew I was becoming a fat slob and I worried I’d end my airline career just becoming a fat slob. And the only thing I did was gain weight. And my blood pressure was starting to rise and rise.
Julie Gregory: Well, that’s because we were eating the diet that our doctors were recommending. We were eating a low fat, high carbohydrate, lots of healthy whole grain diets. And neither one of us was a slouch in any way. I mean I exercised a lot. But I was insulin resistant at that time as well.
Bruce Gregory: Yeah, I was insulin resistant, and I was on a statin, I was taking Nexium and my blood pressure was rising. My neck was getting big enough that they were going to put me in for a sleep study to get a C-PAP machine to carry around. So nobody wants to carry that around the airlines.
Dr. Bredesen: Yeah, and this is one of the things that comes up all the time and it just came up in the trial that we just finished. And by the way nine years ago we had just been turned down for doing the trial that we just finished. So, we tried to do it way back in 2011 and 2012, nine years ago we got turned down. So it was a few more years before we could get anything out. But this comes up all the time, people get off their anti-diabetes drugs, off their statins, off their anti-hypertensives. But Julie let me go to you for a moment. In your incredibly compelling story, I remember it always gets me when I read it about hugging your son who was crying saying mom I don’t want you to die. And coming home to Bruce and saying I think I might be getting Alzheimer’s because I found out I’m APOE 4/4. And Bruce saying to you, “well that explains a lot”. And you just being absolutely crushed because you’re thinking oh my god, he’s not that surprised that I have early Alzheimer’s disease. And you pointed out that he would go on these trips overseas and come back and could see changes even in that short time that he was gone. So then at the same time at the end of your story, talking about you’re able now to see your grown-up son and he’s getting married and all these wonderful things because you succeeded so beautifully. So you two have just been an amazing team. So Bruce just maybe talk about how or maybe Julie talk about how did you get Bruce to jump on your protocol because you were doing a lot of things right. And how did you get your big tough airline pilot, you know CEO type personality to say you know what, I think you’re right, let me get on this with you. And then to go back and actually be showing that the other airline pilots hey this is what you should be doing. So how did you convince him
Julie Gregory: You know in searching on the internet, I came across a lecture that Dr. David Perlmutter gave at NYU entitled “Alzheimer’s Can Be Prevented”. And that was the first doctor I had seen who would make such a bold statement. So I listened to that lecture over and over again. I’d take notes, I started taking the supplements that he recommended. This is way before “Grain Brain”. And at the time he was a practicing neurologist, and I got an appointment to see him. And Bruce came with me on that appointment. And Dr. Perlmutter was so compelling that that was a pivotal moment. From that moment on we gave up all sugar, all grains. We came home from that trip to Florida and we purged our kitchen to the point where at the end.
Bruce Gregory: Oh, it was scary.
Julie Gregory: We looked at each other and said …
Bruce Gregory: There’s nothing left to eat.
Julie Gregory: What’s left?
Bruce Gregory: When you purge everything you’ve been eating for the last 50 years and then you kind of look at it and go well now there’s nothing left to eat so what do we do now, I’m hungry.
Julie Gregory: Yeah, so I think it was Dr. Perlmutter who was so compelling and so convincing.
Dr. Bredesen: Fantastic, yeah David’s done great things. So, Bruce just talk for a minute about what’s been the effect on you? What’s happened to your weight? What’s happened to your health since you’ve been doing this sort of thing with Julie?
Bruce Gregory: Well, typically when you fly international, and then is what I was doing at the time, I was on a triple seven. You would come in for a break and you would drink coffee to stay awake. And the coffee would stimulate my appetite, so I’d eat more of that airline food. And then when you eat that airline food you feel bogged down so what do you do? You drink more coffee. And then you start to feel hungry again because you’ve been drinking coffee so it’s time to eat again. So it was kind of like a cycle and over the years I was getting to be a pudgy little airline pilot. And because of that my blood pressure was going up, I was on a statin. And I was taking Nexium for acid reflux and I just thought I was going to go the way of every other old airline pilot. And it’s kind of sad because you earn all your money in the last part of your career. And a lot of guys end up dying off. If you look at an ALPA study that was put out probably in 1990, if you retired at age 55 you ended up having a normal lifespan at the time which was 83 for men and 85 for woman. But if retire at age 60, you died within two to three years.
Dr. Bredesen: Wow.
Bruce Gregory: What happens in that last part from 55 to 60, aviation ages the hell out of you. I mean it’s just hard.
Julie Gregory: Let’s answer Dale’s question. He’s 30 pounds lighter, he’s all muscle, no medication, no C-PAP machine. And his FAA physician says “what’s your secret you are biologically aging backwards?”
Dr. Bredesen: Yeah that’s wonderful.
Julie Gregory: And all the pilots are all over Bruce trying to figure out what are you doing?
Bruce Gregory: Yeah, because you know you see your friends hobbling because they got arthritis of the hips and their knees don’t work anymore. And when you get to be overweight you get knee replacements, hip replacements, and life becomes quite the struggle. And especially in a sit down job. When historically the best exercise for aviation was to go running. But as you get older and then you’re overweight, you’re hard on your frame.
Dr. Bredesen: Yeah, yeah I know. This is very very helpful thank you. And of course as you indicated so many people go the other way. Oh my gosh my wife has Alzheimer’s, or my husband has Alzheimer’s, and your telomeres go down and your blood pressure goes up and things are really bad. So let’s now talk to Christine and Julie Luby. And you have a really I think a unique perspective here Christine and Julie. Because on the one hand you are health coaches and so you see this from both sides. On the other hand you have been caregivers, you’ve seen this in your own families. And on the third side that means of course that you are at risk yourself. And so you really have a perspective from all these different angles. So maybe you could start Christine and talk a little bit about how you’ve seen this, how this has effected your dealing with your own clients.
Christine Coward: Yeah so, you’re right all those different lenses. You know wanting to do right by myself, knowing my genetic status and risk factors, wanting to do right by my mom who does have Alzheimer’s and got it early and did not know about the Bredesen Protocol. And just I’m actually not her caregiver. But I’m so grateful I have two siblings in the town that she lives in who look after her. And yeah I’m the support from afar with visits. And then just working with people and seeing, you know we did some really interesting groups last year and we’re still doing them, care partner support groups. And seeing the groups that we had that had the care partner, it looks like Julie and Bruce right now in the same Zoom screen. Because the person with the cognitive impairment needed the support of their care partner to be helpful in the meeting and to track and process and so on. And just noticing that the impact sometimes of the caregiver who meant so well by answering for them and just sort of stepping in. And wanting to make them probably look better that way and wanting to be supportive and knowing they could answer the question quicker. You know all those things. And what we know from research that’s out and more that’s coming out is on how much that impacts really the self-esteem and self-efficacy of the person with cognitive decline. Because they’re going to do less and less for themselves and recognize that it’s hard for them. So that’s just one observation and angle to this. And then the other side is self-care. But I want to let Julie Luby talk about it. She’s fresh off of running a care partner support group that we do. And there’s so much wisdom in that room that’s she’s been sharing and so I’ll turn to you Julie.
Julie Luby: Yeah, thanks Chris, there truly is a lot of wisdom in the room and I am just so lucky to be among the care partners that I’m with in the support group. So lots of different things to talk about here. You know one of the really gems of wisdom that was shared was that the care partner recognized that when they stayed calmer, their partner with cognitive decline stayed calmer. And then it was sort of an upward spiral of decreasing anxiety instead of a downward spiral of increasing anxiety. And I thought that was so lovely that they were talking about it in that way. That they understand that how they reacted to the situation, and we choose how we react, actually made an impact on their loved one. And it could make the day better for both of them. And so I just thought that was really wise. You know in my own family my father had Alzheimer’s and he was pretty far into it by the time we learned about the Bredesen Protocol. And my mom was his caregiver. And my mom, if you think about it, they were retired, they’ve been retired for years. In her early 80’s took on this full-time job. And how many of us are really prepared to take on these full-time jobs when we’re in our 80’s? And so it’s something to think about as care partners. You know you’ve got a huge job and it’s a big job, don’t be afraid to ask for help. I find so much of the time my job as the care partner to the care partner was to help my mom navigate. And almost give her permission for yes it’s okay to get help and figure out what do you need help with? And it’s different for every family. Really think about what is that time of day or that activity or something where you just find the most frustration. And how can you maybe bring in some help for that? And I think my job was to really kind of keep an eye on my parents and make sure that my mom’s health, and her mother died of Alzheimer’s, so I have Alzheimer’s on both sides of my family. To make sure that she wasn’t putting herself at risk and that we were keeping her stress level down and finding ways to help her out as she took care of my dad. And so I think that’s really important to think about. And don’t be afraid to bring in help, it’s not the end of the world.
Dr. Bredesen: And could you, having been there could you comment on one thing that comes up again and again. When someone has cognitive change, their immediate feeling is often people will now look at me differently. There’s a whole issue of the stigma that’s associated and therefore they don’t trust themselves. And so they don’t get that positive feedback. They worry that if they just do something that we all do, that people will look at them and say oh my gosh they’re really failing now. And so unfortunately it hastens their own problem because they’ve got the extra stress. Because they’ve got less joy. Because they’ve got less networking and feeling. You know you need to get something essentially to feel. And then of course they’re told don’t even think about improving because it never happens. This is not a disease where you see improvement. So we have to get off all those humps and get over those. And then of course part of it their concern about how their spouse interacts with them and are they being critical? And so we see some people where it helps to have the caregiver reflect positively. And when they look at the caregiver they’re not seeing disappointment and oh my gosh you’re dying and oh my gosh things are terrible. But hey you can actually get better. It is an option. How do you work with the caregivers to have their interaction with the people they’re working with be supportive one? And be one that’s actually going to support new synapses and improving the overall status?
Julie Luby: That’s a great question. And it’s something I think everybody struggles with really in their own relationships with their loved ones to make sure that they do let their loved ones do as much as they can do while they can do it because that does keep them going. I think COVID’s been really hard on some families because there’s been isolation. And I know I’ve talked to some of my clients recently as the world is opening up a little bit and as their loved ones are able to interact with other family. They just really see that helping a lot. And seeing that their loved ones are interacting well with other people kind of brings their anxiety level down too. So I think that’s really helpful in seeing that and getting other people involved in their life. It’s really hard when you call yourself off and you are afraid of the stigma. But that socialization is so important, and I really encourage everybody to do that as much as possible. And find people that your loved one enjoys spending time with and engage those people. Have them help you, have them come over and play guitar with your loved one or sing or whatever might work.
Dr. Bredesen: Yeah thank you Julie. So we’ve got some wonderful comments and questions here so let’s go through. We’ve got some wonderful expertise here on the group in the panel. So Valerie says same statistics as Bruce mentioned for the death for schoolteachers. And sounds like yes school teaching obviously you have very stressful job— no question. And so Bruce when you write your book for pilots, maybe you write a little chapter there for schoolteachers as well.
Bruce Gregory: Absolutely, it’ll be a very simplified book, very direct.
Dr. Bredesen: Yeah, good. And then Laura says there are so many stories just like this including in our family. Misdiagnosis, incorrect approach over and over from numerous specialists. Figuring out on your own through being relentless with research saves lives. Sadly our standard medicate community, a good point, medications first, isn’t taught the correct approach to the body. And absolutely, and I just finished lecturing to some students at a university this morning and absolutely same issue. They’re all taught to write that prescription. And yeah prescriptions are great when they’re doing the right thing, when they’re targeting the right things. But now background on the overall protocol and of course we just posted new results on the clinical trial that showed exactly that this week. Michael says I wish my other four surviving older brothers were listening to this, thank you for the amazing stories, knowledge, and time. Absolutely, thank you, Michael. And yeah for anyone who has cognitive decline, we’re hearing obviously from Christine just a few minutes ago, please, please end it with that generation. Everybody from the next generations should be on prevention or the earliest reversal possible. This should end with the current generation. This should be a rare, rare disease. Valerie says here congratulations on the newest publications. Thank you, great outcome, yes absolutely. And let’s see powered by love. Yes no question there. There is a lot of well-meaningless from that. We’re all trying to get that perfect treatment and that perfect drug. I do think in the long run there’s going to be a combination of precision medicine type protocols. The sort of things that Julie has done extremely successfully and her 3,500 plus members of apoe4.info are doing so successfully with specific drugs. And I think we’re going learn new drug targets. So part of the group I talked to this morning was about developing targeted drugs through an engineering approach. The next one here from Lynette. This is so great to see as I’m preparing to be a certified ReCODE and PreCODE health coach. Fantastic, great idea, Lynette thank you. I too was a caregiver for my mom with Alzheimer’s, I love being aware of these issues. This is something I think it really does; you know it’s taken a village to get through all these things. Sam says I feel totally torpedoed by family that show moms love by offering her diet treats. Yeah so I’ve just been talking to groups that have started and run assisted living facilities. And there’s a wonderful group RALNA, Residential Assisted Living National Association. And then as we talked about Marama before. So absolutely I think that the assisted living groups have to jump in there and start doing the right things to get much better outcomes. And I understand at some point people say it’s just not worth it, I just want to have a bunch of hot fudge sundaes and go off into the sunset. And I think that is an important thing so actually let me throw this out to the whole group here. When someone says to you I just want to have a whole bunch of hot fudge sundaes because that’s what’s left, what’s your response? I mean there’s some validity to that, I get it. And at the same time some of it depends on whether you believe there could be improvement. So what do you all say to people who say that?
Christine Coward: It so depends on their stage. I think it’s of course not a great idea because we all know what sugar does. And there’s a reason why when Julie met with Perlmutter that they went off sugar because that’s impactful. And there comes a time where somebody might be pretty far along and it’s a tough kind of battle to fight that pleasure seeking habit when it’ll be tough to get support from the care team in an institutional living.
Dr. Bredesen: Yeah absolutely. Yeah, and Julie Gregory, I know you’ve had family members where this is an issue. And obviously you serve as a wonderful role model. But what do you tell people who say look the doctors are just telling me that there’s nothing I can do? What do you tell them?
Julie Gregory: I share my story to break the stigma. We have to normalize cognitive decline and getting better. Because I think it’s more frequent than anyone knows. I mean, I think we see this on apoe4.info all the time. We see people who do the wrong thing and do badly. And start doing the right thing and they feel better. And when you get down to the ice cream sundae, if the person’s in the early stages, ask how do you feel after you eat that? I feel really bad after both dairy and sugar. So it’s a really good idea to pay attention to the signals your body’s giving you. There’s nothing wrong with an occasional treat. But the fact is we can enjoy treats now made with healthy ingredients that taste almost the same.
Bruce Gregory: Actually better.
Julie Gregory: Actually better, yeah. And you feel good afterwards.
Dr. Bredesen: And I actually think you know we were talking about this recently about with residential assisted living leaders. And the issue there is everybody wants something that tastes good. So if you can just change the game by saying hey you can actually do the right things and we can supply you with things that actually are good things that you’re not sacrificing happiness. Then we’ve won the war, that’s going to be everything. As long as people say I’d rather have a hot fudge sundae and I just don’t care anymore, we’re going to have people and we see this all the time. You go, you’re having a little trouble and then you go into assisted living facility and whom straight down because everything is wrong. You’re getting drugs to control the behavior, you’re eating wrong, you’re sleeping wrong. You’re depressed understandably, everything is tough. But if we can now have people do better, they have more times with their loved ones. And some people will now come back out of the facilities. And then we’ve really made a big impact. So I think Marama down in San Diego with Dr. Heather Sandison is a wonderful example of a place that’s doing just that. And Heather is reporting that nobody there is getting worse so it’s fantastic to hear that. So let’s go on to the next one here and let’s see here. Di says we need to spread the word as much as possible. Couldn’t agree more, this is something that’s critical. Nikki says I’ve been anxious for most of my life, LCSW so a social worker treated anxiety for a living. Yeah so our daughter does the same thing and I have to say I couldn’t do her job for three days. It is so stressful. You’re dealing with some of the most difficult situations in the world. And so she says how does one address APOE 4/4 and not feel stressed? Well I think you look at Julie and say, “wow she is doing well” and I suspect Julie’s going to do well and Bruce until they’re 100. So that’s the future, this should be a rare disease. Nobody should have this problem. Nikki says I’m 47, relatively good weight, eating a Keto diet, good for you. Probably too many animal products. Okay yeah and as Julie’s pointed out, please get on a plant rich, mildly ketogenic diet with appropriate fasting and appropriate high phytonutrients and high fiber and all the things that she’s done. And she says it feels stressful to take supplements and do all these things. So yeah good point. And it’s stressful just thinking what’s my future? So please I think again reading Julie’s story and other stories from people who have done very well, take it one step at a time. We are trying now with the recent trial to make things simpler, to take it in phases. And so maybe Julie, both Julies, could you weigh in on what do you say to people who say I want to do the right thing but that in and of itself is stressful.
Julie Luby: It is, I mean I would say that I do work with people on mindset. And really helping them to think about what is their why? Why do they want to be healthy? Why do they want their health? Why do they want to live another 5, 10, 15, 20 healthy years? Because sometimes when we can come back to that then it’s a little easier to make changes in your life to do those things. And I think what I saw too is as you make the changes, as you stop eating sugar you don’t miss the sugar as much. In fact things start tasting really sweet. And I don’t think people believe that when they get started that they really are going to change. So I think I can talk about sort of thing with them. And we also, we don’t want people to be stressed. So we find out what’s the most important thing. And when we work with people as coaches, there’s a couple ways you can go about it. Some people really do well when you find the low-hanging fruit and they can make a couple of easy changes and see that it’s not so hard. And then other people want to dig into the hardest thing. They are like I’m going change my diet tomorrow. And we have to work with them. They have to kind of determine their path because that’s the way they will be successful.
Dr. Bredesen: Yeah, and Julie Gregory maybe you could comment. What do you say to people who say I want to do what you’re doing but it’s too stressful for me?
Julie Gregory: You know it might feel that way at first when you envision making all these changes at once. But you don’t need to make all these changes at once. It’s just baby step after baby step after baby step. And with everything you do you feel so much better that it become self-perpetuating. Like I wouldn’t miss exercising every day for anything because I feel so much better when I do it. And that in and of itself is a stress release. And for me it’s spending time in nature, I always exercise outside no matter what the weather. And that’s an amazing stress release. Following protocol is a return to an ancestral lifestyle. And so, when it starts to get dark outside I’m asleep. And when the sun comes out, I’m awake. And everything has an ebb and a flow, and my life right now is very easy and not stressful. So over time it becomes that way, but it starts with baby steps. And I think it depends on the individual, but you don’t need to make all the changes at once.
Bruce Gregory: If you look at it more as just having a habit pattern for one item. And when that habit patterns established it’s part of your life like breathing air. And then you can grab another item and make that too a habit pattern. And that’s kind of what you’ve been alluding to. And it’s easier than making all the changes all at once.
Dr. Bredesen: When we make optimal protocol easy and fun for everyone, that’s when things will really turn around. Because people worry about oh my gosh is it going to be a problem? And here’s another example. So Kim asks help, can we indulge in some sugar? How bad it is to have it occasionally? I say sugar Sundays but don’t know it’s that’s too frequent. So certainly there’s no question a lot of people cycle out of ketosis once or even twice per week. Often the recommendation is to do it with a little sweet potato or something. So the question is yeah, how bad is it to have a sugar Sunday? So, Julie do you ever have a sugar Sunday?
Julie Gregory: Oh no, I don’t have any desire for that because I know how I would feel afterwards. And I guess the answer depends where you are on your journey. I think as a APOE 4/4 who’s had a history of cognitive decline, I have to be extra careful. But if you’re a young person and your risk isn’t as high as my risk, maybe sugar Sundays are okay. I think it really depends on what your risk is. But I would still say you can find that same dessert that you’re craving, and you can make it in a healthful way
Dr. Bredesen: I would recommend get a CGM, get a continuous glucose monitoring, stick it on yourself for a week or two weeks. And then do your sugar Sunday and see what happens. And look if it barely bumps you at all and you keep a good HOMA-IR at your next checkup, you probably are just fine. On the other hand if you go from fasting of 85 to 200 you’ll know that you’re really hurting, especially if you now crash and drop down to 45 and have poor sleeping and things like that. It really hurts you at both ends of the scale. Then you can see for yourself what it’s doing. The next one is from Veslina, I’m 30 years old now, my grandmother had Alzheimer’s, mother with early onset dementia. Today I got my genes tested, unfortunately I have not only APOE4 but others too related to neurocognitive issues. I’ve already started with the protocol to prevent anything to happen. Really thankful for the book, got familiar with the work. So fantastic yes please it’s perfect timing. You now know you have some risk and again this should be a rare disease, please get on it. And as Julie said, take it one step at at time, you can continue and as Bruce was pointing out, you can do it that way, a little bit at a time. Melissa says why won’t the Alzheimer’s Association work with you to find the cure. Yeah great point. And I think we’ll get there. I think at some point there will be interest in that. To some extent there’s lots of funding from drug companies and it does take some time to change that around. I do think that when the drugs and the protocol is working together, that’ll be something that everybody gets, and I think we’re heading in that direction. But there’s no question, we are saying what’s been done for so many years has simply been wrong. The research has kind of not understood what needs to be done. We’re saying here, here are all these people who are getting better, how come you guys aren’t doing that? So it is tough to hear that what you’ve been working on for years has not helped people and someone else is claiming that they are. But over time these things change. This is what happens with medicine, medicine is about tradition and permission. It’s not like Silicon Valley about disruption. If you look at the history of scurvy, the treatment for scurvy with Vitamin C was found every century for several centuries. They’d find it, some people would get better, the medical community would reject it and people would be dying for another 100 years. I mean it’s a horrible story. The same thing of course happened with germ theory. And so Dr. Semmelweis who himself died of germs because they forced him to go into an insane asylum because he was claiming that he could help people. So this is the history of medicine. It will take time, but things will change. Next one is Jan says with Wheat Belly in 2019 my 92 year old mom came off eight to nine treatments, some toxic meds. Even though she cheats occasionally with I’m too old for this she’s remained off all of those meds, fantastic. As we were talking about earlier, most of these medications, they’re trying to cheat nature if you actually look to see. So when you have hypertension, the question is not where can I get a prescription for antihypertensive? It’s why do I have hypertension? And let’s figure out why you have hypertension and then let’s get rid of the reason that you have hypertension which is often standard American diet and lifestyle. All right Laura says our digestive system is our first brain, yes very good point. Tremendous enteric nervous system there as well. Hippocrates understood this, mess up the gut, mess up the brain and the entire body no question. Metal, mold, toxins and of course so now we’re all living in an Alzheimer’s soup. Genetics, epigenetics especially regarding detox pathways, sleep, absolutely and daylight. And Julie you mentioned the daylight in your eyes absolutely. This is a great point. Grounding, bare feet, all of these are critical. Toxic outdoors, toxic indoors yes. All of us who have been in the Californian fires know how toxic the outdoor can be at times. So no question these are critical things and now we can actually follow these biochemically to see who’s succeeding, who’s not succeeding. And of course that was what was done in the trial. Mary says just saw a video of the mayor of New York offering free hamburger and French fries for anyone who gets the vaccine. Yeah and of course the vaccine is critical right now and people are doing anything possible. But no question as we’ve talked about before, the pandemic we’re just coming up on 600,000 Americans who have been killed. Probably within the next week we’ll hit 600,000. The number of the currently living Americans who will die from Alzheimer’s is almost 100 times that many. About 45 million of the currently living Americans. So it is a pandemic that is much, much larger than the COVID-19 pandemic which is why it’s important for all of us to get on the right prevention and early reversal. Shawn says thank you all of you for what you do. I understand the science in protocol but how does one persuade an aging relative with MCI to take things seriously, any insights? Yeah please get on apoe4.nfo, take a look at all the wonderful people and what they’re doing. Please check in with Christine and Julie Luby and all of the people who are seeing results. And please check out the publications because ultimately data show what’s actually happening. Valerie says such enlightened sessions covering so many wide issues. God bless you and continue always, thank you very much. Mike asks how do I become a coach? Christine can you tell Mike about that?
Christine Coward: Yes and I love that Mike, we need more coaches working in this space. What we don’t offer here at Apollo Health is the foundational training that you would need. So we recommend a national health and wellness board certified approved program such as Functional Medicine Coach Academy so check them out. And once you complete that, then you’re a certified coach. And to be an Apollo Health ReCODE certified coach then you would take our course. But you don’t want to take our course until you’ve had some foundational coaching background.
Dr. Bredesen: Thank you very much Christine. So and let’s take a couple last here. Nicole, might this have a significant impact in patients in their 90’s who are quite sociable and active despite advanced age and despite moderate cognitive decline? Absolutely we see it all the time. We’ve had examples of people with MoCA scores of zero who have improved no question the earlier you start, it easier it is. But we do see people who are even in later stages. So I’m very interested in a future trial which we would called the SARA trial, severe Alzheimer’s reversal attempt, we’ll see. But no question people who have SCI, all of them get better. MCI, most of them we can see some improvement. Full on Alzheimer’s some of them we can see improvement. So yes please, and again some people will do it, some people won’t. But please get them seen by someone who knows what they’re doing. And then Donna asks could you do the Mediterranean instead of the keto diet? So the one issue there is the Mediterranean diet does not get you into ketosis. And again when we say keto diet we’re talking about plant rich ketogenic diet, not a lot of bacon. And so maybe Julie Gregory could you talk about people who are on apoe4.info. Are they doing Mediterranean diet and are they doing things that don’t include ketosis? Certainly theoretically including ketosis is a big help.
Julie Gregory: I think that’s true. And if you think of KetoFLEX 12/3 which is a diet we recommend as being the Mediterranean diet without grains. Because essentially we’re eating all the other components so it’s very, very similar. And of course there’s amazing pasta substitutes now like pasta from the hearts of palm and from almond flour and all sorts of other things. So if you absolutely need that pasta. But the diet’s really very, very similar. On apoe4.info we have people probably doing a variety of different diets. I do think most of the people in our community understand the importance of ketosis. Because we as early as age 20 have this deficit in fuel going to our brain. We can’t use glucose efficiently. So APOE4 carriers especially benefit from being in ketosis whether it’s through diet, fasting, exercise, or a combination of the three.
Dr. Bredesen: Yeah you know the more that we study this disease the more we realize that the fundamental nature of this problem is a brain subsystem deficiency. There’s deficiency, whether it’s oxygenation, whether it’s blood flow, whether it’s nutrition, whether it’s tropic factors, whether it’s because of too much toxicity or pathogens and too much inflammation. It is a deficiency in supporting this critical network. And this is where ketones definitely help. So what we’ll do, let’s take the rest of the questions online. Thanks very much to everyone for absolutely great questions and comments. And thank you so much Bruce and Julie and Christine and Julie, thanks so much for your expertise and for all the great things you’ve been doing.
Bruce Gregory: Thank you.
Julie Luby: Thank you.
Dr. Bredesen: Thanks guys. Everyone stay safe, take care.
Julie Gregory: Bye-bye. Dr. Bredesen: Bye.